This was created as a question and answer page for anyone with dental questions. Dagon H.C. Jones, DDS used to check this page periodically and answer general questions about dentistry that anyone had. This page now exists only as a resource of information. Dagon Jones is no longer actively monitoring this page and posting responses.
The advice and information given here are strictly for entertainment purposes only. Please understand it is impossible for any health care provider to diagnose or treat any condition via a wiki or any other online source or other media. For the most accurate information please visit your family health care provider whether dental or otherwise. That said, it is an entertaining note that questions are usually answered by dentists within the community. But legally, it's entertainment, got it?
This page is intended for questions about dental procedures, dental science, and dental materials, but not for questions about billing and insurance. Questions about billing and insurance should be addressed to your dentist's office or insurance company.
Questions about fluoride? See Water Fluoridation Information about Xylitol can be found on the Xylitol page.
Other dentists in the community are welcome to respond to questions as well.
- If you have other questions, ask the wiki!

Medical Professionals are limited by HIPAA as to what information they can make public about their patients, including who their patients are. As such it is very hard for Doctors, Dentists, and Psychiatrists to respond to negative comments on the wiki. Please keep this in mind while reading any comments. |
2008-04-18 08:07:17 This page has been here for a while, someone must want to know about dentistry. Am I the only one that thinks this stuff is cool? —DagonJones
2008-04-18 11:06:01 Okay, I will ask something. I need to get a bridge because I am missing tooth #4. What is the procedure like? How long does the bridge last? What can you tell me about cost? —CalamityJanie
Options for Replacing Missing Teeth

 Implant 2008-04-24 15:25:56 Well first off you have several options for replacing a missing tooth. Usually the best option is a dental implant. After a tooth is extracted the bone in the area will slowly resorb or dissolve away because the bone no longer receives a chewing stimulus from the root of the tooth. This often does not pose a problem for maybe 25-35 years. A dental implant will maintain the density of the bone in this area because it acts like a tooth root. An implant is intended to be permanent, they have only been around for about 25 years but all research suggests that they will last for the life of the patient if properly cared for. Implants have a very high success rate (around 97% in the #4 area). A single implant is often only about 15-20% more expensive than a bridge. A bridge is used to replace a missing tooth by placing a crown on each adjacent tooth with a false tooth (called a pontic) in between the two crowns. I usually only recommend a bridge if the two adjacent teeth would benefit from crowns. It is unfortunate to have to shave down healthy teeth to make a bridge. Having said that a bridge can be an excellent way to restore a missing tooth. They feel natural but because the three teeth are now fused together you will not be able to floss normally between them and you will need to use a special tool called a floss threader to clean under the bridge. Bridges tipically last 15-20 years but can often last much longer if done well and cared for. Eventually the bone around #4 may resorb away enough that the existing bridge does not look very nice anymore and needs to be replaced. Or the bone resoprtion may (this is rare) compromise the adjacent teeth. A bridge is often billed out as the same as 3 crowns, so the price in Davis may be anywhere from $2400-3200 depending on the materials used and the dentist. A bridge takes at least 2 appointments, one to prepare the teeth for a bridge and place a temporary (This appointment can last 1.5-2.5 hrs), then you will have to return in 2-3 weeks to have the custom lab made permanent bridge cemented (0.5-1 hr appointment). An implant will likely cost about $3500-4200, once again depending on the dentist and materials used. An implant is a more involved process than a bridge and often takes 4-7 months before it is completed (this assumes the extraction site of #4 has completely healed). Ussually another doctor, typically an oral surgeon or a periodontist, will place the implant and your general dentist will restore it with a crown. The whole process takes 4-5 apppointments most of which are very short and painless. Hope this helps, I am happy to answer other questions you have. —DagonJones
Implant 2008-04-24 15:25:56 Well first off you have several options for replacing a missing tooth. Usually the best option is a dental implant. After a tooth is extracted the bone in the area will slowly resorb or dissolve away because the bone no longer receives a chewing stimulus from the root of the tooth. This often does not pose a problem for maybe 25-35 years. A dental implant will maintain the density of the bone in this area because it acts like a tooth root. An implant is intended to be permanent, they have only been around for about 25 years but all research suggests that they will last for the life of the patient if properly cared for. Implants have a very high success rate (around 97% in the #4 area). A single implant is often only about 15-20% more expensive than a bridge. A bridge is used to replace a missing tooth by placing a crown on each adjacent tooth with a false tooth (called a pontic) in between the two crowns. I usually only recommend a bridge if the two adjacent teeth would benefit from crowns. It is unfortunate to have to shave down healthy teeth to make a bridge. Having said that a bridge can be an excellent way to restore a missing tooth. They feel natural but because the three teeth are now fused together you will not be able to floss normally between them and you will need to use a special tool called a floss threader to clean under the bridge. Bridges tipically last 15-20 years but can often last much longer if done well and cared for. Eventually the bone around #4 may resorb away enough that the existing bridge does not look very nice anymore and needs to be replaced. Or the bone resoprtion may (this is rare) compromise the adjacent teeth. A bridge is often billed out as the same as 3 crowns, so the price in Davis may be anywhere from $2400-3200 depending on the materials used and the dentist. A bridge takes at least 2 appointments, one to prepare the teeth for a bridge and place a temporary (This appointment can last 1.5-2.5 hrs), then you will have to return in 2-3 weeks to have the custom lab made permanent bridge cemented (0.5-1 hr appointment). An implant will likely cost about $3500-4200, once again depending on the dentist and materials used. An implant is a more involved process than a bridge and often takes 4-7 months before it is completed (this assumes the extraction site of #4 has completely healed). Ussually another doctor, typically an oral surgeon or a periodontist, will place the implant and your general dentist will restore it with a crown. The whole process takes 4-5 apppointments most of which are very short and painless. Hope this helps, I am happy to answer other questions you have. —DagonJones
2008-04-25 10:30:09 Thank you for the detailed explanation Dr. Jones... I have been undecided between an implant and a bridge... I guess I thought a bridge would be much cheaper but it seems to have its downside if it doesn't last as long. And I also agree that it would be a shame to pare down the teeth so drastically on both sides of the missing tooth. When I saw illustrations of that online, it made me kind of sad, I just can't explain it. I had a periodontal procedure about 2 months ago, and Dr. Shirazi presented me with the opportunity to just have the implant done at the same time but I chickened out, and at the time, I still thought a bridge would be better. Well, I guess I can go back. I have braces currently but he said he has barely enough space for the implant to be placed. —CalamityJanie
2008-04-25 10:46:39 You are very welcome. If you are currently wearing braces, you most likely have the opportunity to move the teeth to make more room for an implant, talk to your orthodontist and have your orthodontist and Dr. Shirazi discuss the options. Of course there are other options for the missing #4, including doing nothing (which I dont recommend because the adjacent teeth are likely to shift into the open space). Other options are limited to different types of removable appliances that you would have to take out at night. Most people dont prefer removable appliances but they are more cost effective. —DagonJones
2008-04-29 14:39:37 I've got two main questions. The first is regarding the effectiveness and the relative radiation exposure between conventional film based x-rays vs digital x-rays. The next is regarding "Diagnodent" and similar laser based tools. I just don't know much about what this can be used for, and am wondering if it might be something I'd be interested in.
Thanks for setting this page up, and thanks in advance for any feedback,
2011-08-23 Dr. Jones. First off, thank you for all of your help yesterday. You have a new patient long-term patient now. I have been reading this page and, since I had my tooth-root extracted on my last visit, was wondering if I should consider saving up for the implant to replace the now missing root/tooth or if it is something I would be functionally fine without. I don't want a bridge in the future but seeing the information here about receding bone structure gives me a bit of pause for thought... Should I, or anyone else, be worried about this? — Wes-P
Digital X-Rays and Radiation exposure
2008-05-01 13:56:57 Great questions because I know there is a lot of “buzz” about digital x-rays (radiographs) and laser caries detection. First off lets discuss x-ray films, dental x-ray films come in 3 speeds, D, E, and F speed. F speed is the most sensitive speed and therefore requires less radiation exposure than the other two films. “Results reported in literature illustrate that switching from D to E speed produced a 30-40% reduction in exposure. Switching from E to F speed produced a 20-25% reduction in exposure, and switching from D to F-speed film produced a 60% reduction in exposure”. The above quote is from an article by the FDA located here F speed film is newer and therefore more sensitive, there is little difference in image quality between D, E, and F speed films. Most modern dental offices that do not use digital radiographs use F speed film. I don’t know the exact reduction in radiation exposure by switching from F speed to digital radiographs but I have heard it reported that the difference between D speed and digital is a 90% reduction. So the difference between F speed and digital is probably 20-30% reduction. In my opinion (which is shared by most dentists I speak to) conventional film produces a clearer image, which makes diagnosing decay easier. However digital films are much quicker, easier to transport, provide the option of digital manipulation, and have slightly less radiation exposure to the patent. Some newer digital sensors have very clear images which are comparable to traditional films. Approximations of the radiation dose received by different medical exams relative to global averages and acute exposures can be found on this Wikipedia entry.
The radiation exposure from a full mouth x-ray series (approximately 18 films) is roughly equivalent to the same exposure the average global citizen receives during two to five days of daily life (background radiation exposure from cosmic radiation, radon gas, etc). I consider the difference in radiation exposure between F speed film and digital radiographs small enough that it is not significant. A full mouth series is only taken about every 5 years, typical dental screening films (bitewing x rays) that are often taken every year have the equivalent of about 1 days exposure of background radiation.
Diagnodent and Shallow Decay
Regarding laser caries detection I will discuss the Diagnodent because it is the only device that I am familiar with and understand the technology. Similar devices exist on the market but I cannot comment on their effectiveness. A diagnodent works by shining a laser into the pits and grooves of a tooth to detects bacteria. Many oral bacteria have molecules in their cell membranes that fluoresce (give off light) when exposed to a particular wavelength of laser light. The Diagnodent measures this fluorescence and gives a number reading and an audible tone. More bacteria produce a higher pitch on the audible tone and a higher number readout. The instrument is sensitive enough to detect small levels of bacteria that do not need a filling so the number readout is important. A number of 30 or above has definitely broken through to the deeper part of the tooth and needs a filling. Numbers from 20-30 are questionable and depend on the visual presentation and the patients decay risk, therefore these are left up to clinical judgment. I have been very surprised by how deep some decay is that otherwise looked and felt normal on the surface. Heavy and dark stains in the grooves of the teeth are an indication of possible decay.
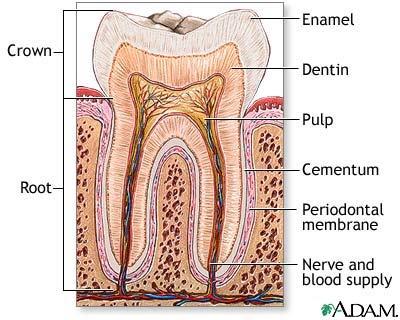
When decay is shallow and in the enamel only it is reversable. Ions from your saliva can absorb into an early lesion and remineralize the affected enamel. Fluoride and other agents can aid this remineralization process. This generally only works on the smooth surfaces of the teeth (like in between the teeth and on the sides). When decay is very shallow on the chewing surfaces of the teeth it often continues to spread despite all best efforts to keep the areas clean. This is because all the pits and grooves of the teeth harbor many bacteria and are difficult if not impossible to clean. Access to decay in the pits and grooves of the teeth is often straight forward; therefore, removal of only the decay with a very small preparation (hole) can be achieved. This is often referred to as "microdentistry". So if your dentist tells you you have cavities ask if any of them are possible to remineralize. Remineralization can be assisted by fluoride mouthrinses and xylitol chewing gum. Xylitol is a natural sweetener that inhibits bacteria from sticking to the teeth. The most important aspect of remineralization is preventing acid attack, so brush and floss daily (flossing is ussually the key) and avoid frequent sugar/charbohydrate snacks. Once decay has grown past the enamel and is into the dentin (the inner part of the tooth) a filling is necessary. If you are attepmting to remineralize some very suspicous areas of decay your dentist may want to take x-rays more frequently to make sure they dont spread too deep.
The Diagnodent is a great tool to help detect decay that is lurking deep in the pits and grooves of the teeth that would otherwise not be detected. However it is just a tool and the dentist has to understand its limitations. A Diagnodent cannot detect decay in-between the teeth and cannot be used next to an existing composite (tooth colored) filling. A Diagnodent will give a false positive if there is heavy plaque or tartar in the grooves so those grooves need to be clean. Also if a Diagnodent is used after a cleaning and the hygienist has used any colored agents (special toothpaste or plaque staining dyes) the Diagnodent may get a reading from the pigments in the dye and give a false positive. Remember that just because the Diagnodent is giving a reading, does not mean that there is decay that needs a filling. I hope this info was helpful and I am happy to answer other questions. I would not let digital radiographs or use of a Diagnodent be a deciding factor when choosing a dentist. There is a lot of new technology in dentistry but none of it is a replacement for good clinical judgment, skill, and compassion.
2008-11-09 15:40:27 Great page, Dr. Jones. My question isn't about dentistry exactly, but more about low-cost dental services in Davis. Are there low-cost options for dental care in Davis, e.g. for those without coverage needing a filling? —robinlaughlin
2008-11-10 10:08:25 If you are a Yolo county resident and meet certain income requirements you can go to the Davis Community clinic "Communicare Heath centers" which is behind sutter hospital. There are 4 Communicare dental clinics in Yolo county, Davis, Woodland, West Sacramento, and Esparto. The Davis dental clinic is open Tuesday-Friday. 530-757-4667 call for more info. You will need to go into the clinic and fill out an application. They also accept Medi-Cal. If you are having an emergency you can come in at 8am or 1pm (sharp)for an emergency appointment, there is no guarantee you will be seen that day but if there is enough time you will be taken care of. I volunteer there once a month on Thursday nights so you may see me there. Communicare is a good resource but they are underfunded and have such a huge patient base that there is often a very long wait for appointments. Be prepared to provide documents to prove your residence in Yolo county and your income.—DagonJones
2009-05-17 22:20:45 My teeth have severe enamel erosion. The tips of my front teeth seem a bit translucent, and they're very sensitive. I want to find a way to remineralize, however there are two different ways that are confusing me. The first says to use toothpastes like arm and hammer enamel care with ACP. This also contains fluoride, and glycerin. I've heard that glycerin will coat the teeth, and prevent remineralization. The second method is to use all natural, fluoride, and glycerin free toothpastes. Right now I'm trying the Green Beaver brand. This has silica, and sodium bicarbonate, as well as vitamin C, which they claim helps strengthen teeth, and gums. Which of these methods is the correct way to remineralize? Does glycerin containing toothpastes really inhibit remineralization? Which would nullify the benefits of ingredients like liquid calcium, xyitol, and novamin. —bluevelocity
2009-05-18 13:16:45 I do not know if glycerin inhibits remineralization. Logically, I dont see how it could, because if it does leave a film on the teeth, it would be a water soluble permeable layer. The teeth naturally form a permeable protein layer on top of them called the "pellicle", minerals can freely move through this layer to remineralize the tooth surface. To address your question more generally, I dont think remineralization will help your problem. Remineralization refers to restoring minerals to demineralized enamel, this changes the enamel from being weak and soft to hard and durable. However, remineralization can not restore lost tooth structure or rebuild lost enamel (not to a visible extent, only a microscopic one). When acid (either dietary or from bacteria via carbohydrate metabolism) attacks tooth structure it pulls out minerals (demineralizes the tooth). Your own saliva is very good (better than any toothpaste) at providing a super saturated environment of minerals to help remineralize demineralized tooth structure. If demineralized tooth structure suffers a prolonged acid atack it will be destroyed, ussually resulting in a cavity.
You can address the sensativity by using a sensativity protection toothpaste, like sensodyne, but these often do not work all that well. You can use a professional product (only available through a dentist) called MI paste. This is the one product that may be better at remineralization than your own saliva. It prevents sensativity by blocking the microscopic tubules that are in exposed dentin. It can be applied at home and needs to be used for several weeks but generally has very good results.
Regarding the translucent incisal edges, if the enamel is very thin on those teeth you may want to consider having tooth colored composite filling material bonded on to the edges to reinfoce them. Or you can have the thin edges "sanded" off by a dentist. —DagonJones
2009-05-18 15:17:26 Floss first, and then brush; or brush first, and then floss? —TheAmazingLarry
2009-05-21 11:59:47 So, I usually wake up with a thick almost gummy white film on my teeth. Is this plaque or is it this "Permeable protein layer"? —MasonMurray
2009-05-21 19:17:43 The film on your teeth in the morning is definitely plaque, you cannot feel the pellicle, it is only a few microns thick. According to the reseach I have read and how I was taught in dental school, it does not matter what order you brush and floss. But it is VERY important that you do floss daily.
- From what I've heard, not flossing allows bacteria to build up just under the gum line, and the gums retreat downward, away from it. Can that retreat reverse itself over time with proper brushing and flossing? And another question: does mouthwash make a difference for anything other than bad breath? I've heard that too sterile a mouth can leave the door open for thrush.
2009-05-21 19:42:25 Plaque is a bacterial biofilm. It's what you gotta take care off every day. If you don't, it'll eventually lead towards cavities and mineralize up to turn into calculus/tartar, which brushing won't remove (but your dentists sharp thingies are meant for). —EdWins
Periodontal Disease
 health on left, periodontitis on right
health on left, periodontitis on right  Recession on left, normal on right 2009-05-22 23:15:28 Periodontal Treatment is the key to a healthy smile! By taking care of your gums, you can avoid gum disease and keep your smile looking its best. Periodontal Treatment offers a variety of products and services to help you achieve and maintain a healthy smile. Periodontal treatment is a form of dental care that focuses on the gums and other supporting structures of the teeth. Periodontal treatment can help to prevent the progression of periodontal disease and can also help to restore the health of the gums. Drleilazamani
Recession on left, normal on right 2009-05-22 23:15:28 Periodontal Treatment is the key to a healthy smile! By taking care of your gums, you can avoid gum disease and keep your smile looking its best. Periodontal Treatment offers a variety of products and services to help you achieve and maintain a healthy smile. Periodontal treatment is a form of dental care that focuses on the gums and other supporting structures of the teeth. Periodontal treatment can help to prevent the progression of periodontal disease and can also help to restore the health of the gums. Drleilazamani
Your smile is one of the first things people notice about you, so it’s important to take care of your teeth. Good oral hygiene habits are important for everyone, but they’re especially important if you’ve had periodontal treatment. Periodontal disease is an infection of the gums and bones that support your teeth. If it’s not treated, it can lead to tooth loss. Drleilazamani
After you’ve had periodontal treatment, it’s important to take care of your teeth to help prevent the disease from coming back. Here are some tips for taking care of your teeth after periodontal treatment:
1. Brush your teeth twice a day with a soft-bristled toothbrush.
2. Use toothpaste that contains fluoride.
3. Floss your teeth every day.
4. Visit your dentist regularly for professional cleanings and checkups.
5. Quit smoking. Smoking is a major risk factor for periodontal disease. Drleilazamani
The reason flossing is so important is that it removes the plaque between the teeth that brushing alone does not. This plaque can lead to cavities between the teeth or gum disease. The area between the teeth includes the area below the gum line that is between the teeth, also known as the periodontal pocket. This diagram shows a health pocket on the left and a pocket with periodontitis or periodontal disease on the right. Because the pocket area is a low oxygen (anerobic) environment, lots of nasty bacteria can breed there. Over time they produce lots of toxins, your body responds by producing inflamation (redness, swelling, bleeding etc.) Both the bacterial toxins, and your body's own response causes attachment loss, where the gum tissue attachment point migrates downwards, this creates a deeper pocket which is harder and harder to clean and can harbor more bacteria. the presence of attachment loss in the pocket area is ussually the diagnosis of periodontitis. As the gum tissue attachment point migrates downwards, the bone will follow becuase it always wants to maintain a certain distance from the gum attachment point. Periodontitis can result in rececession, which is when the gums visibly move downwards exposing the root surface. There are many other causes of recession, such as vigorous tooth brushing with a hard or medium bristle toothbrush (always use soft or extra soft, they clean just as well) some recession can come with age. Once recession has occured it can only be repaired with a gum graft. The proper treatment for gum disease is scaling and root planing (aka a deep cleaning) this is where tartar and bacteria are removed from below the gumline with specialized instruments (your gums are ussually numbed up for this). Ussually some of the gum tissue will re-attach to the root surface after the scaling and root planing, but because the bacteria can migrate back into these areas, periodontal maintenence cleanings are ussually recommended 3-4 times a year. It takes about 3 months for bacteria to build up the colonies and enviornment required to cause progression of gum disease. Even if there is no re-atachment to the root surface, if there is a reduction in the inflamation, then the severety of the disease has been reduced. —DagonJones
Regarding mouth washes, there are a wide variety of mouthwashes that are designed for different purposes. Some, like Scope, are just to freshen breath. Others, such as ACT or Fluoriguard have fluoride and help prevent cavities. Listerine helps fight gingivitis and gum disease. There is a prescription mouth rinse that kills bacteria responsible for decay and gum disease. I have never heard of mouthwash leading to thrush (or Candidiasis) but I can see the logic behind that because if the micro organism ecosystem in your mouth is disturbed it can allow Candida, a fungus, to proliferate and take over leading to thrush. However, I wouldnt worry about mouthwash causing thrush, I think that is pretty unlikely.
Wow great questions you guys, this is fun!
2009-05-23 10:15:40 Hey, out of curiosity and since you like the questions, here's a family medical oddity. My father's family is prone to never getting some of their adult teeth or getting them very late. My grandfather was x-rayed over and over during WWII by dentists because they were curious about it. I still have some teeth that never changed (premolars, and thankfully they look fine), I didn't get my second molars until I was in my mid 20s, and my wisdom teeth came in (straight and true) five years later. My father and his siblings all have some of their original teeth as well. As a side note, we're all pretty durn cavity free, other than my brother who lost all his baby teeth for adult teeth and had his molars come in at the usual times. I've always wondered how common this is. Have you run across it before or have you ever heard of it? —JabberWokky
- You're definitely not alone. My family has this oddity, too. I still have some baby teeth, and my father had a baby tooth removed in his 40's. —JessicaLuedtke
2009-05-28 12:48:00 It is very common to have congenitally missing teeth run in families. There does not seem to be any specific pattern, like skipping generations, mother's side of the family, or anything like that. However, it is most commonly bicuspids and lateral incisors that tend to be absent. Ussually people do just fine with the baby teeth but sometimes they will fall out becuse they have shallow root structure or they can also start to resorb (melt away) which may necissitate an extraction. Regarding your second molars (aka 12 yr molars) comming in late, that sometimes happens but to the best of my knowledge it is not related to the congenitally missing teeth. —DagonJones
2009-05-28 18:49:35 Even stranger, I actually had a 3rd set tooth try to come in. I had it surgically removed because it was not properly formed, but my great-grandmother had the same thing.... Odd how it sometimes skips... er... 3 generations? —MasonMurray
2009-05-30 19:17:40 Question: My 6 year old sons "upper right lateral" baby tooth was knocked out @ Kindergarden running around—this was in October. Anyhow, we had it x-rayed and the dentist said we will have to see what happens. The "upper left lateral" tooth fell out and it's just emerging through now. I'm thinking then, his upper r. lateral would also be emerging around this time; but it's not. I felt both sides of his gums and on the right, it feels and also looks like it tooth is kind of stuck up there?? It doesn't feel the same on the left. Is there anything that can be done if the tooth is not coming down? —JRaumer
2009-05-30 22:33:07 I have a temporary crown right now and will get it replaced with a permanent one in a week and I was wondering how durable the permanent crowns are. —hankim
2009-05-31 22:04:46 JRaumer: Your son's tooth is likely to be just fine. the contralateral (other side) teeth rarely come in at exactly the same time, they are often seperated by about 6 months or so, sometimes longer sometimes less. If a primary tooth(aka baby tooth) is knocked out then there is potential for damage to the developing adult tooth, but this is very rare and unlikely. If it looks and feels like there is a tooth under there then he is probably in very good shape, often times there is a very pronounced tooth shaped swelling for several months before the adult tooth finally erupts through the gums.
hankim: A permanent crown is genarally designed to last a lifetime, however, there are many things that can cause a crown to need to be replaced. Decay, excessive wear, tooth fracture, can all necissitate replacement. The average ( and this is a very rough estimate) life of a crown is about 20 years. depending on why the tooth needed a crown in the first place plays a big role in the long term life span of a crown as well. If the tooth had very extensive decay or has a root canal then the life expectancy is less. —DagonJones
2009-06-10 18:01:11 I have a few questions about kids and teething: At what age should youngsters start going to the dentist? And, how do foods affect dental and jaw development throughout the deciduous teeth period? ——related to this last question, I've heard that eating lots of HARD foods (granola, etc) as a kid will result in straighter and stronger permanent teeth later on. Is there any truth to that? —TheAmazingLarry
2009-06-11 13:12:05 Children should see a dentist by age 1. When kids are very young we do a visual exam to check for signs of decay or other oral health problems. We also review proper brushing and flossing techniques for parents, discuss fluoride, diet, etc. from ages 1-5 I ussually recommend an exam once a year, unless the child has a high risk for decay then I recommend every six months. I have never heard of hard foods leading to straighter and stronger teeth, and I cant see how they could. This sounds like an "old wives tale" to me. The position of adult teeth can be influenced by the position of the deciduous (baby) teeth; however, the chewing forces on the baby teeth would have no effect on the development or position of the adult teeth. Tooth development can be effected by systemic factors like a very high fever or certain medications such as tetricycline (which causes gray stains on teeth), but indirect forces would not effect the cells responsible for tooth formation. Heavy chewing forces could lead to more dense bone around the baby teeth because bone is a very dynamic tissue and is responsive to physical forces. Bottom line is hard foods are not needed or recommended for proper tooth development.—DagonJones
2009-07-16 14:01:07 One of my teeth-premolar upper has slight split from one side. Is is straight down split. It doesn't bother me much except I eat too hot or too cold. My dentist was suggesting me to have a drill and fill it. I am very much cautious about my teeth and I am afraid to do the drill thinking that it will make my tooth worse coz my dentist was saying that she will make a horizontal drill and make up the split portion with fill. I am also scared that while making a horizontal drill on my teeth, she may be hurting my next teeth adjacent to it. I would like to get your opinion- Shall I go for Drill and Fill or just let it stay and avoid eating hot and cold stuff.
Sorry for the late reply. I doubt your adjacent teeth will be harmed by the drilling, if it is a vertical crack on the cheek side of the tooth it would be very hard to damage the adjacent teeth. For most fractures I would actually recommend a crown as opposed to just a filling. If the tooth is sensative to cold, and sensative when you bite down then the tooth almost definitely needs a crown. Fractures in teeth can spread pretty easily once established and they can lead to cusp fracture or sometimes root fracture. If there is a fracture in the root, then the tooth will need an extraction. It is very hard to say without actually examining your tooth, but I would not recommend doing nothing. If the tooth is sensative and there is visual signs of a fracture you should definitely have the tooth repaired. —— dagonjones
2009-08-27 19:21:29 My son is 14 years, 11 months. All his teeth have come in and he is currently in braces. His canines came in late (left canine just finished coming down two months ago) and space had to be created with springs to open room for them. Right now, his right maxillary second molar is primarily retained but the oral surgeon said it should have been exposed much sooner and now he should just wait as it probably won't come down after being exposed. There seems to be nothing in its path and the other three second molars came in fine. Could this be related to tooth b being extracted at 10 years old due to a cavity? Is it likely the second molar will come in after being exposed? —Genny
It would be almost impossible for the late/hindered eruption of a second molar to be related to an extraction of tooth B at age 10. The second molars do not replace any primary ("baby") teeth, therefore, it would be very difficult to damage the developing tooth bud of a second molar during an extraction of a primary tooth. By the way primary tooth B is replaced by the upper right first premolar (#5). Delayed or hindered eruption of second molars does happen sometimes, this can happen for a variety of reasons but often it is difficult to know why. Sometimes they can be moved into proper position with braces but that can sometimes be difficult. I would discuss the case with his orthodontist, ask him directly how likely it is this tooth will come into proper position. —- dagonjones
2009-09-09 11:34:57 I have a question. For all of my life, I've had a tiny black dot that appears to be a tiny hole of some sort on the top of one of my molars. It has never bothered me and I've never had a dentist say a word about it. Should I be concerned about it? —ChristyMarsden
2009-09-10 11:33:41 That tiny black dot is probably one of the pits or grooves that are very common in molars. if the pit is deep enough it can pick up quite a bit of stain. Most likely it is only staining and I would not worry about it, especially if you get regular exams. Sometimes those stains can have decay underneath them, a diagnodent (see above) is a good tool to see if there is decay there but ussually it is not necissary becuase the decay can be detected during a standard exam. —DagonJones
2009-09-10 17:57:26 I had a new crown molded a month ago, and the permanent gold one has been in for two weeks now. Would this change be enough to cause me to start biting the inside of my cheek when I eat? I started noticing this once I got the permanent crown put in, and today I started really feeling out the area where this is occurring, noticing that the "real" tooth above the freshly crowned one seems to have some deep gouges on the sides. Now this may have been there from a previous filling-I can't really tell as it may be a tooth colored filling, but it did seem like my dentist drilled on the upper tooth while the lower was being prepped for the crown. Did I imagine that, or would there be a legitimate reason for the dentist to do that, OR is the dentist looking to "guarantee" future revenue down the line when I might need a filling or another crown on my last natural molar? —CFletcher
I am going to give some quick answers and hopefully come back to put in more detail later. It is relatively common to adjust the opossing tooth during a crown preparation, this ussually does not damage the tooth but could make it feel a bit rougher, it can be polished if need be (ask your dentist next time you go in). When two teeth meet togeather there is an ideal amount of overlap that prevents the cheek from getting caught between. that can change a bit when a crown is made, it may not be the dentist or labs fault but rather simply the limitations that are present when making a crown. I have encountered this situation a few times, ussually the body adapts and the person "learns" to stop biting, if it is very serious the crown may need to be replaced. I have met many people who have a cheek biting problem with natural teeth with no crowns or fillings. -dagonjones
2009-09-13 17:40:29 Hi Dr. Jones,
On my last appt, the doctor kept calling out 3's, 4's and a few 5's. He said I had "calculus" and needed a deep cleaning. From what I have had described, the deep cleaning will open up the underside of my teeth to the outside permanently. And, because of this I will be stuck going back 3 to 4 times a year. This frightens me because it 1) opening me up to the outside world sound like it will do more hard than good and 2) since I do not have the ability to go back 3 to 4 times (or ever once a year), if I have this done and can not keep going back over and over and over I will be really, really screwed. Please tell me I am wrong? What do you recommend? -T —ToddAndMargo It sounds like you have periodontitis (gum disease) see the above entry :2009-05-22 23:15:28 Peridontal Disease for more info about gum disease and its treatment. Calculs is just another word for tartar, it needs to be removed because it is like a playground for bacteria. The deep cleaning will only remove bacteria and calculus from the tooth root. It will not expose any part of the tooth to the outside that was not already exposed. I think you should really commit to cleanings at least 3 times a year (even if your insurance does not cover all of them), and the deep cleaning (root planing), it can really make a big difference. The long term results of gum disease can be tooth loss, also untreated gum disease can increase your risk of cardiovascular disease, stroke, and type II diabetes. The 3's are not bad and the 4's are marginally bad, the 5's are definitely indicate the presence of gum disease, but it is not just the numbers but the severety of the inflamation present in the gums. Inflamation is indicated by redness, bleeding, and swelling of the gums—dagonjones
2009-09-13 17:56:20 Hi Dr. Jones,
I lost a lower front tooth in a car accident about 40 years ago. I have a lot of bone loss in the empty space. If I can ever afford an implant, I will need bone replacement. Can this be done with ACP (amorphous calcium phosphate) or similar? Or, am I stuck with surgery?
If surgery, where do they get the bone from? And, what effect will stealing the bone have on the site where it was stolen from? -T —ToddAndMargo
Bone is ussually deminieralized cow bone or human bone from a tissue bank, both of which have NO risk of transmission of disease. If bone is harvested from your own body (which has the best chance of success but also the most uncomfortable) then the donor site will take a while to heal and ussually hurt but it will heal just fine in the end with almost no chance of permanent damage. The bone would ussually come from your leg or your jaw. The bone graft is considered surgery, but you will not likely need surgery to harvest bone becuase most bone grafts today use material from a tissue bank. —dagonjones
2009-12-02 10:12:08 My molar broke last night (on a Tues). A piece of it the broke off and seemed to crumble. I left a message for my dentist, but alas, her office is closed on Wednesdays. I'm flying out of town on Friday. What's a person to do? —NoelBruening
Her office doesn't list an emergency / cell phone number? My dentist does, so you might want to check.
No number given. —Noel
If your dentist does not leave an emergency number just find a dentist who is available that day, Davis is full of great dentists who would be happy to help you out. Most dentists will do a temporary fix for you to last you long enough to get back to see your regular dentist.
This situation of a cracked tooth is a very common problem. It often happens around older amalgam (silver metal) fillings. Some amalgam fillings have sharp internal line angles that can be a stress point for a fracture to begin. ussually a cusp or wall of the tooth will break off leaving a sharp edge and exposing the senative dentin. These situations are ussually not a significant emergency, the most likely symptoms are irritation to the tongue from the sharp edge and sensativity to touch and cold from the exposed dentin. Dentin is the inner part of the tooth underneath the enamel, it has millions of microscopic tubules that can carry a pain impulse into the nerve of the tooth. Having the dentin exposed does not put the tooth at immediate risk for other problems, if left exposed long enough (months) the dentin is more likely to get decay. Teeth with fractures like this will ussually need a crown to restore the missing tooth structure and protect the tooth from further fracture. If the dentist does not have time to do the crown that day, they will ussually put a temporary filling material in the void to cover the sharp edge and sensative dentin. Thanks for the questions and keep 'em comming. -dagonjones
2009-12-21 09:10:23 I have a worn out gold crown on a back molar. A couple of local dentists said they would replace it with a $450 stainless steel crown. Other say pretty much over their dead body, but would not give a reason. One says stainless is stronger and last longer, they just look bad. Since it is too far back to see, I do not care. Is there some reason to stay away from stainless and pay the $1100 for a gold crown? —ToddAndMargo
2009-12-22 10:09:24 I would strongly recommend against a stainless steel crown. Stainless steel crowns are pre made and come in a variety of sizes, none of which will provide a precise fit for your tooth. Stainless steel crowns often (almost always even in the hands of great dentists) have very rough margins. These rough margins collect plaque and tartar and often lead to decay in the long run. A custom crown is made in a laboratory and should have a very smooth margins with a precise fit that will not allow bacteria to accumulate. If cost is a big issue just keep the gold crown you have, if there is a hole worn through the top a small filling can be put there. This filling may not even be necissary if there is not decay present. Talk to your dentist and find out if the crown absolutely needs to be replaced, it may be able to be patched. A stainless steel crown will be more expensive in the long run because it will not last as long and is much more likely to lead to decay. Stainless steel is a stronger material than gold but the metal is much thinner on a stainless steel crown than a gold one. —DagonJones
- Dr. Jones, I have had dentists tell me that gold is the best filling material (or the best material for onlays/inlays or crowns) because it wears the way a tooth wears, adjusts to changes in temperature, and is the least likely to make your tooth crack. And that they last the longest. The downside is that it is not all that attractive. Do you agree with all of that? —CovertProfessor
Yes I would agree with your dentist's statements. I love gold, it is definitely the best material for onlays/inlays and crowns. Gold restorations are the strongest and most conservative (that is they require less removal of tooth structure). Porcelain requires more removal of tooth structure because it needs to be thick to be strong. Gold also has the smoothest margins (tooth to restoration transition). But they are not natural looking so I usually only recommend them for posterior teeth. I love to admire gold restorations in teeth, I have seen many that are over 40 years old. -dagonjones
Thank you — that is helpful! —CovertProfessor
2009-12-22 16:24:58 Hi! Lately I have had a lot more tooth sensitivity (cold and hot) in the back of my mouth, one molar on the right side of my mouth. I have a filling there, not too old...am wondering if this is something I need to be worried about? I brush and floss, no bleeding or pain from that anywhere...Thanks! —jsbmeb
2010-01-05 15:34:18 Your sensativity to cold could be many things, It could be a cracked tooth, infected nerve, decay, or nothing at all. Teeth are often sensative to cold, and this can change with time. Teeth with fillings are more likely to have sensativity but even perfectly healthy teeth can have transient sensativity. I would wait several weeks, your cold sensativity will likely subside with time and it may even come back in the future. If it continues to get worse or if the pain is severe and lingers for more than one minute after the cold is removed you should see a dentist. —DagonJones
Wisdom Teeth or 3rd Molars
Wisdom teeth often need to be extracted because there is simply not enough room for them in the jaw. The definition of impaction is a tooth that cannot erupt fully into the mouth. Sometimes wisdom teeth erupt fully but are in a problematic position and need to be removed. Even if the tooth is not painful or obviously problematic it may require extraction. Impacted wisdom teeth often push against the teeth in front of them and can lead to decay or resorption (biologic destruction). Wisdom teeth extraction can be done under light sedation or general anesthesia (being put to sleep) or no sedation, in all situations the areas are thoroughly numbed so there is little or no pain. Minor swelling is common and often not visibly noticable, very large swelling (like a chipmunk) is infrequent and often the result of an infection but is often easily treated with antibiotics. Pain is usually minor to moderate and often lasts for about 3-5 days and is managed well with prescription pain medication. - Dagon Jones
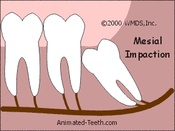 2010-01-06 10:15:20 Hi Dr. Jones... This problem has been bothering me for years—I have a impacted wisdom tooth in my lower jaw (mesial impaction? as seen here except it is fully erupted):
2010-01-06 10:15:20 Hi Dr. Jones... This problem has been bothering me for years—I have a impacted wisdom tooth in my lower jaw (mesial impaction? as seen here except it is fully erupted):
I had already spent quite a lot of money a few years ago getting oral surgery to lift and straighten it, but it failed. I've been keeping it clean and so far by flossing and brushing excessively and have not had any cavities in the impacted area yet, but often times I get pain in my jaw and pressure-build up and aches...
I was wondering what my options are? Can it be fixed, or must it be removed? If I get it removed, will I need to remove the corresponding tooth on the jaw above it (I'm reluctant to remove one tooth, yet alone two)? Thanks in advance! —H4rry
2010-01-14 08:55:24 What you are describing is probably "pericoronitis" which simply means inflamation around the crown. It is a common problem with lower wisdom teeth. because the gum tissue sits very high around the tooth plaque, bacteria and food often get caught below the gum and lead to infection, inflamation and pain. The best solution is almost always to remove the tooth. The inflamation can be treated every time by topical antibiotic rinses or debridement (cleaning under local anesthetic) or sometimes recontouring of the gum tissue. I would not recommend these methods because the problem will ussually continue to recur.
You probably will eventually need to have the upper tooth removed as well because after the lower tooth is removed the upper will tend to hyper erupt, which means it will drift down because it does not have a tooth to oppose it. The soreness and pain could be due to TMD (temporal mandibular disorder AKA TMJ) but is most likely from the wisdom tooth. If you get the tooth removed you probably will not miss it, you will be able to chew just fine, and it will be easier to keep the adjacent tooth clean. If you are fearfull of the procedure you can have general anesthesia or deep sedation. I hope those answers help. —DagonJones
Thanks Dr. Jones. I've just gotten SHIP insurance through UCD and would like to get that partially-erupted-tooth-in-question removed—does your office offer oral surgery for that removal, or do you have a referral for an oral surgeon? Thanks! —H4rry
We do most oral surgery in our office; however, if the extraction is very complicated or if general anesthesia is requested we refer out to a local oral surgeon. Best thing to do is make an appointment for an evaluation and we can asses the tooth and make a recommendation based upon the situation. —DagonJones
2010-01-20 19:43:58 I have two questions. I got braces when I was ten and had them for three years. But once I got them removed I didn't use my retainer because it didn't fit properly, it would pop out. A couple of years later when I went to a different dentist, I was told that because I had braces at a young age the root of my two front teeth are short and weak. My first question is, can getting braces at an early age really do that to the root of the tooth and is the effect reversible? My second question is, because I stopped using my retainer right after the removal of my braces, I have crooked teeth again. I want to get braces again, preferably a removable aligner, but will it further damage the roots of my front teeth? And thanks in advance. —XuJeong
2010-01-25 22:49:09 During orthodontic movement the roots of teeth can become resorbed. It is more likely for this to happen when the teeth are being moved very rapidly (which was not likely the case if you were in braces for three years) , but it can occur during regular orthodontic movement. Unfortunately the effect is not reversable. It is possible to move your teeth again with braces but the chances of further resorption are present and depending on the severety of your resorption it may not be recommended. You would have to check with an orthodontist. The orthodontist would evaluate your x-rays and the severety of crowding and let you know how significant the risks are.
I emailed this question to Dr. Molitor (a local orthodontist and all around nice guy) here is what he had to say:
"These are good questions. There is no evidence that braces at an early age causes increased root resorption. As a matter of fact the opposite seems to be true. That is, orthodontic treatment on the very young rarely produces root resorption. It is true however that orthodontic treatment for younger kids often implies prolonged or multi-phase treatment which can be related to increased risk of root resorption.
For those that have already experienced root resorption, further orthodontic treatment definitely can be risky. The decision to do orthodontic treatment is always a balance of risks and benefits so it would depend on how much the teeth need to move, how much root is left on the affected teeth, and how much the "crooked teeth" bother you. "
Hope that helps. Matt Molitor
2010-02-03 12:45:23 Any advice for somebody about to see a dentist (for a cleaning) for the first time in over 20 years? I've never had any problems (straight teeth, including wisdom teeth that came in fine and are accessible for cleaning, never had a cavity, etc), but I figure there might be some questions I should ask or something like that. Other than some back of the tooth staining from coffee and tea, I have no issues I can even think of. I should also add that I don't have any fear of dentists at all; I have just been a business owner for many years, and I didn't have dental insurance until I got married, and then didn't think about going until my wife pointed out that with our upcoming move, we'll be changing insurance, so I might as well take advantage of what we've been paying for and go now. —JabberWokky
2010-02-03 20:28:06 Very informative page. I have been considering a dentist but will need time to consider it, however, partly due to personal interactions and partly due to seeing the extremely positive reviews I think I would definitely have visit Dr. Jones. —WesOne
- Indiana Jones? —hankim
2010-02-03 21:24:40 JabberWokky; when you see a dentist make sure they check your periodontal (gum) health. This step is known as perodontal probing, it involves the dentist or hygienist feeling your gums and counting out a series of numbers. See the entry on this page dated 5-29-2009 for more details. If it has been a long time between cleanings there is likely a good amount of calculus (tartar) buildup on your teeth, which has likely led to inflamation or even gum disease (lets hope not). Dont feel swindled if the dentist wants you to come back for 2 or more cleanings, if there has been tartar on your teeth for more than 20 years it can be very hard to remove and sometimes it takes longer than 1 hour to get it all. If you have other questions after your first visit let me know, you can email me the x-rays and I will be happy to review them and give you my advise. —DagonJones
2010-02-09 10:52:57 What's your general feeling on sealants? I was always a very good brusher and had no cavities until late college. In high school my dentist insisted on sealing my teeth, which my mom (a former hygenist) was not very happy about because she feared they'd eventaully crack and leak, thus trapping things under the sealant. Given a sudden onset of cavities (probably 10 surfaces in 4 years) with no other changes in brushing, flossing, or visiting a dentist, is it possible the sealants were not such a hot idea? Thanks in advance. —AmLin
Sealants
2010-02-09 14:15:13 I recommend sealants based on the risk of decay for the tooth. If a person has a history of decay and the tooth has very deep pits and grooves, then a sealant is a very good idea. For kids under 10 sealants are usually recommended on the adult molars because kids commonly have a higher risk for decay (love of sweets and lack of good brushing). For a good sealant the tooth must be kept very dry during placement, if moisture gets on the tooth during the sealant process the sealant won’t bond well and it could leak. The grooves should also be very clean, it is best to clean out the grooves with a very small drill, a microblaster ( a very small sandblaster), or a spinning brush with pumice. If a sealant is placed well it will last a long time and the risk of getting decay under it is very slight. If a sealant is not bonded well then plaque can get under the seal and lead to decay. If decay is sealed in under a sealant when the sealant is placed, the decay won’t spread (if it is completely sealed) because the bacteria can not get a carbohydrate food source. Overall, sealants are a very good thing; they do much more good than harm. However, they can be a problem if they are not sealed well but this is usually rare.
Regarding your situation, I have seen a lot of college students who had a long history of cavity free checkups. But when they are in college they all of a sudden have multiple areas of decay. These are usually in between the teeth and due to a lack of flossing and/or a change in diet (frequent snacking on carbohydrates or frequent consumption of sugary beverages). Also there can be a change in the oral bacteria during this time of life as people start new relationships. Oral bacteria are spread via kissing and people can acquire different bacteria that are better at producing acid; therefore, better at producing cavities. It is hard to say if your cavities were caused by the sealants. If you can get your dental records look to see if the fillings were in-between the teeth (they will say DO or MO or MOD). If they are in between the teeth then they are not related to the sealants. If the fillings were occlusal fillings (records will say “O”) then they were put on the chewing surface of the teeth where there may have been sealants and could have been related to leaking sealants. I hope that helps.
2010-02-09 15:57:09 I have a cap on one of my upper molars, about two years old. Part of the cap is metal (amalgam, perhaps? not gold). Normally it doesn't bother me, but when I swim in the pool, sometimes I get an uncomfortable "metal" feeling. Any idea what could be causing that? Chlorine? Exercise? I'm clenching my teeth while swimming? Should I be worried about it? —CovertProfessor
2010-02-09 19:47:34 The metal is most likely noble white gold. Similar to the white gold in jewelry. It has a silver appearance in is commonly used in porcelain fused to metal crowns (aka caps). The sensation you are feeling is probably due to clenching your teeth while swimming, I would try to avoid that. Too much force on teeth can cause sensitivity. I would not worry too much about it, it is very common for teeth with dental work to be a little sensitive from time to time (this even happens on teeth with no dental work). I would only worry if it was painful very often (like once or twice a day) or if it started to get increasingly worse. —DagonJones
- Thank you, that's helpful. You're surely right about it being noble white gold; I'd remembered that it was supposed to be gold, but when I looked at it, it didn't look gold, so I got confused. And I will try to stop clenching while I swim. :-) —CovertProfessor
2010-02-20 15:04:50 Is it possible to induce temporary sensitivity via a ton of sugared candies? —StevenDaubert
- Tooth sensitivity can be tricky, many things can cause it and it can be very transient. Teeth can be sensitive to sweets, especially if you have areas of deep decay or exposed dentin. I would say yes, it is possible, but it is not a commonly known cause of sensitivity. -DagonJones
2010-02-20 15:44:36 About four years ago I had corrective jaw surgery to fix an open bite. Now my jaw regularly locks and has to "pop" open, which sounds like a loud crack. Is this a normal complication from the surgery, or is it potentially unrelated? —MHaymond
TMJ/TMD
TMJ refers to the TemporoMandibular Joint itself and TMD refers to TemporoMandibular Disorders.
- It is probably related to the surgery but this type of thing happens in many people who have had no surgery. The jaw joint (Temporomandibular Joint AKA TMJ) is a rather complicated joint. There is a fibrous disc between the two bones and this disc can slip in and out of position resulting in a loud pop or click. The jaw can also get locked open or closed because the jawbone can be forced into normal depressions in the base of the skull. Because you have these joint noises you are more likely to develop pain and discomfort of the joint or jaw muscles due to regular strain/ stress on these structures. However, you may never develop pain. So, don’t worry about it if it does not hurt. If it does hurt, you should see a dentist. DagonJones
The following is a general list of recommendations for jaw pain (TMJ/TMD):
- Wear your bite plate (night guard) every night during sleep. Your bite plate is designed to reduce clenching and grinding as well as position your jaw in its most relaxed and stable position. (Bite plates are made for people with chronic TMJ pain)
- Use alternating hot and cold compresses on the affected muscles or joint when you experience discomfort. Alternate hot and cold every 3 minutes and end with cold. Ice wrapped in a washcloth can be used for a cold pack. A sock filled with rice and micro waved for 1-3 minutes can be used as a hot pack.
- Take Ibuprofen 800mg (4x200 mg tablets) every 8 hours (three times a day) for 1 week. This dose will reduce inflammation in the muscles and joint. (use this dose for moderate to severe pain, this is a prescription strength dose and should only be used under supervision of a physician or dentist.)
- Take Ibuprofen 400-800mg as needed for pain. (mild to moderate pain, doses above 400mg are prescription doses and should only be used under the supervision of a health care practitioner.)
- Avoid hard or chewy foods. Avoid any activity that can overwork the jaw muscles such as chewing gum or prolonged talking.
- Reduce and manage stress in your life. Stress often increases habits such as nighttime clenching or grinding of teeth, which can make jaw pain worse.
2010-02-22 11:19:59 So years ago... I got into a pretty bad car accident. Ever since, I've had this jaw popping thing happen whenever I open my mouth big to yawn or the like. It's as if the right side of my jaw unhinges itself and slides to the side ever so slightly. Never caused any pain, but lately I've been waking with an ache on that side. How do I fix that? —Aaron.Curtin
-
Oh goody, lets go into more detail about how the jaw works. The TMJ is a unique joint in that it actually goes thorough two different types of movement; Rotation and Translation. When you first open your jaw, the joint rotates in the socket (like a hinge). Then during the second part of opening the mandible actually dislocates from the socket and translates down the base of the skull. The fibrous disc that I mentioned above sits between these two bones to lubricate and aid this movement. Trauma can tear muscles or fibrous ligaments that attach to these bones or surround the ligament.
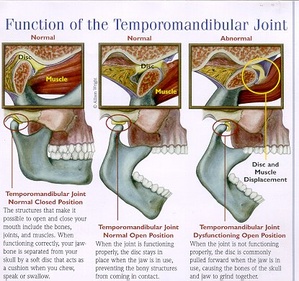 left shows rotation, middle diagram shows translation
left shows rotation, middle diagram shows translation
What probably happened to you Aaron is that one of these muscles or ligaments on the right side was torn and did not heal exactly the same as before. So now when you open on the right side the disc slips out of position (resulting in a pop or click). Also your jaw may be translating further on the right side resulting in your jaw moving a bit to the left. The pain you are having on the right side in the mornings is likely due to night time grinding or clenching of your teeth (aka parafunctional habits). These movements can create a lot of stress and strain on the muscles and the joint, resulting in soreness. I would guess that you have had an increase in stress in your life (stress often makes jaw discomfort worse). You could try some of the things listed above (minimize stress, minimize hard/chewy foods, thermal compresses). If your symptoms persist or get worse you should see a dentist, it would probably be best for you to have a custom bite plate made. DagonJones
2010-03-18 14:10:10 During a recent exam I was asked what my daily regimen consisted of: brushing, flossing, etc. One tool that came up that I'd never really thought about was a water pick. I don't use one, and never really thought about using one. I brush and use mouthwash at least twice a day, floss once a day, and have no problems with my gums. Is there any reason to use a water pick as part of a normal daily routine? I've always thought of them as somewhat gimmicky or for people with specific issues. —JabberWokky
2010-03-18 14:23:38 Also during the recent exam, they brought up some non-tooth oriented items. For instance, the fact that my jaw sometimes locks open when I open my mouth really wide (usually in a big yawn), and usually clicks when I open it wide. There's no pain unless it locks, and it happens so seldom that I consider it a non-issue. You've answered the question about the jaw clicking already (although they think mine is because the tendon slides over a bone causing transition). But the question I had after leaving was: how far does the practice of dentistry go beyond teeth? I've always considered it a tooth and gum field. Since they measured my jaw displacement, obviously the jaw hinge is also a common part of the field. Are there any other common non-directly-tooth related problems that one can see a dentist rather than a doctor about (or at least bring up during an exam)? —JabberWokky
That is a pretty good question. Treatment and diagnosis of TMJ disorders is covered in most dental schools and is certainly an important aspect of dentistry because it can often be directly related to how the teeth fit together. Some dentists pursue further training in TMJ disorders as well as chronic pain disorders relating to the head and neck. Another aspect of dentistry that is not directly tooth or gum related is oral pathology. Oral pathology is actually a recognized specialty of dentistry (while things like cosmetics and implants are not). Oral pathology deals with diseases that manifest in the oral cavity, it is often dentists who diagnose or first see these problems because they look in the mouth more than any other health care practitioner. It is not ethical or legal for a dentist to diagnose or treat conditions below the head and neck. One might consider dentists "mouth and jaw doctors". Many Oral surgeons have both an MD and a DDS degree (such as Dr. Tomaich). These specialists most commonly perform extractions but are trained in any and all surgeries of the head and neck. They often are called in for hospital trauma cases, and they can perform cosmetic surgery as well. —DagonJones
2010-03-18 14:26:39 As a third, semi-rhetorical question, is there anything that people commonly do that is worse to the overall health of all parts of your body than using tobacco? —JabberWokky
I would want to refer you to a pathologist about that. However in my opinion tobacco is about as bad as it gets, tobacco seems to have a negative effect on just about every organ system. —DagonJones
2010-03-18 16:34:13 If there's only a root, is there another option other than root removal? —BruceHansen
I would have to see the situation; however, there is rarely anything (good) that can be done with just a root. A root canal could be performed on the root then it could be used for retention of a partial denture. —DagonJones
2010-03-22 11:58:29 a week ago i awoke with a sore throat. turns out it was strep and i was put on antibiotics thursday. however, the day prior (wednesday) i noticed some gum tenderness while brushing, which turned into gum bleeding and lots of tenderness/redness of the gums by thursday afternoon & friday, through to today. it would seem to be gingivitis, but i was too ill with the strep to do much about it other than continue to brush and use some listerine. my question basically is: do you think i need to get in to see a dentist asap (i'm out of dental insurance for the year due to a wisdom tooth extraction a few months ago) or, since this was likely triggered by the strep, will continued brushing etc clear it up in time? —RyanJames It is hard to say what is causing the problem, if you don't have a toothache then it is most likely gingivitis. If there is any pus coming from the area see a dentist ASAP (it could be an abscess). If it is gingivitis the best thing to do is brush well (not hard, but thorough), floss, and use listerine. Gingivitis is caused by bacteria and should get better if the area is kept clean. If it does not get better in a week I would go see your dentist. —DagonJones
2010-03-22 16:18:00 With no intent to create a debate, I will ask a very simple question: Is dental coverage included in the new health care bill? —JabberWokky
- My understanding is no. However, it "authorizes early funding of community health centers in all 50 states (Bernie Sanders’ amendment). Community health centers provide primary, dental and vision services to people in the community, based on a sliding scale for payment according to ability to pay." I suppose it helps expand on the Health Centers Initiative success. -ES
* I love your debate disclaimer. I don't think it provides for any dental coverage (I have heard of nothing). I have not followed the bill closely, I was going to wait until it was all finished to figure out what it says. My understanding is that even Canada does not have any public dental care despite their renown public health system.
2010-03-24 12:56:16 Can eating too much citrus be bad for the teeth? Grapefruit was on sale at Safeway for the past week, and I’ve been eating 1–3 a day… last night while brushing my teeth felt a bit more sensitive than usual. —EBT
Yes, citrus can be damaging to teeth. Citrus fruits are very high in citric acid, that is what gives them the sour or tart flavor. The acid can dissolve the minerals in tooth structure. This can make teeth more sensitive but most often people don't notice any discomfort but the erosion can be seen on the teeth. Lemons are the most acidic and people who suck on lemons often have severe acid erosion on their front teeth. I love oranges and eat a ton of them when they are in season, it is usually not a problem. The best thing to do is avoid keeping the fruit in contact with the teeth for prolonged periods of time, enjoy in moderation. Eating a bunch of grapefruit for a week is not likely to have long term significant consequences, most likely the acid has removed a thin protective layer of calcium that covers any exposed root surfaces. This will often make these rooth surfaces sensitive. Try using a sensitivity protection toothpaste for a few weeks and the sensitivity will likely go away. —DagonJones
2010-04-19 20:19:13 What is the cost to replace a crown on a molar? —shilee91
2010-04-19 21:48:24 A typical crown in Davis costs $800-1000 (regardless of the tooth it is on). If you have insurance, most insurance companies will pay for 50% of the cost. Let me know if you have more specific questions. —DagonJones
2010-04-19 21:56:20 Besides brushing at least twice a day and using flouride and Listerine, what's the best way to get rid of stains around the gum line and between teeth in the time between dentist visits? I read somewhere to brush with baking soda, but then I also read that that's really bad for the tooth enamel. —MonicaWilliams
There are not many home products that remove stains well because it does require a fairly abrasive compound to do so, try using baking soda with dental floss to get the areas between the teeth, use an up and down motion while pressing against each tooth. For areas at the gumline use a brush with baking soda. Baking soda is best used once a week because it is fairly abrasive, I would not consider it bad for enamel but using it daily could cause excessive abrasion. —DagonJones
2010-04-29 01:48:12 I must confess... I'm afraid to go to the dentist. My parents took me up until I moved out, I went once since then, and I have been avoiding dentists altogether for like 3 years now. Bad, I know. I am having tooth pain now so I know I need to make an appointment soon, but I have a question that may or may not help me feel better about going. I am cavity-prone, I get cavities all the time. Why is it that whenever a dentist sees a cavity they have to stab that sharp hook thingy into it and cause me immense pain? If you can see the cavity there already, is it really necessary to jab it? I am cringing just thinking about it now. I know I will have cavities next time I see a dentist so I think this is why I hate it so much. —JenniferCook
This is actually a very good question. Caries (cavities) are diagnosed primarily by feel, not sight. Dark areas in the pits and grooves of the teeth may be heavily stained and not carious. An instrument called and explorer (that little hook thingy) is used to feel these areas to find out if they are soft or hard. If the tooth structure is soft, then it is decayed. This should not hurt but sometimes people have very sensitive teeth or deep areas of decay and it can be painful (I do this daily and only get a painful response about 1-2% of the time). Some areas of decay can be deep within the grooves and below the level of the explorer and wont be detected by feel. To find decay in these areas a diagnodent can be used to detect decay. When you see a dentist, ask them to use a diagnodent (call the office to see if they have one) or be gentle and only feel the area if they have to, sometimes the decay is so obvious by sight that feeling it with the explorer is not necessary. No one will be offended and no one will think you are a wimp, we see people every day who are nervous, anxious, and afraid. Don't be hard on yourself about not going to the dentist in the last few years, many other people are in the same situation you are. Your dental team is there to help get you back on track with proper oral care, not scold you for what you did wrong. —DagonJones
2010-06-06 16:30:05 I have several root canal treated teeth, yet everytime my dentist close the canal with the plastic pin. I get a swelling under the tooth. One molar he already extracted because he said it was unsavable. Can a systemic disease be causing the swellings I am experiencing after he close my root canal treated tooth. Thank you
I have never heard of a systemic disease causing recurrent infections in root canal treated teeth, however a compromised immune system can make them more likely to occur. Root canals are not always successful, sometimes they become reinfected and need re treatment or sometimes extraction. I am not sure what you are talking about when you say close the canal with a plastic pin, perhaps you are referring to the "gutta percha" which is a rubber based material used to seal the canals, can you tell me a bit more? —DagonJones
Root Canals
 Infected Pulp
Infected Pulp  Cleansing and Shaping
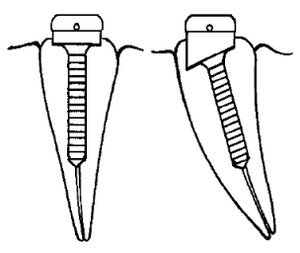
Cleansing and Shaping  Sealing with Gutta Percha This is an excellent opportunity to talk about root canals. A root canal (or Endodontic [endo = inside, dontic = tooth] treatment) is performed when the pulp chamber inside a tooth becomes infected. The pulp chamber is the hollow area inside a tooth that houses the nerve and blood vessels. The nerve and blood vessels enter the tooth through a very small hole at the base of the root (see image at the very top of this page). The most common reason for infection of the pulp is bacterial contamination due to decay, a cavity gets deep enough that it penetrates the pulp. Once the pulp is infected, the immune system cannot bring enough blood flow through the small portal at the base of the tooth to supply an adequate immune response to heal the infection. The tooth must either be extracted or the all the nerve and vascular tissue must be removed from the pulp space. Removal of the tissue within the pulp space, sterilization, and subsequent sealing of the canal space is what a root canal consists of. A root canal begins by removing all decay and providing a clear access hole to the pulp chamber and canals. The canals are then cleaned and shaped using small files. Cleansing refers to removal of all bacteria, nerve and vascular tissue. Shaping refers to widening the canals to remove potentially infected tooth structure and allow adequate room for the filling material. During the cleansing and shaping process the canals are rinsed and sanitized using a diluted bleach solution (all of this is done with a rubber dam to prevent the bleach solution from entering the mouth). Once the cleansing and shaping of the canal is completed the canal is dried and filled with a thermoplastic (softens when heated) material called gutta percha. The material is heated to soften it and it is condensed into the canals so that is fills in all the space, sealing cement is also used to further assure all spaces are filled and sealed. The root canal is now finished and a permanent restoration is needed to fill in the space created by the decay and access cavity. Root canal treated teeth often require a crown to help prevent fracture. Root canal treated teeth have a much higher risk for fracture because they have often lost a considerable amount of tooth structure due to decay and the access cavity. A root canal can become re-infected for a variety of reasons. If the canal space is not cleaned out thoroughly or if it is not adequately sealed a re-infection is more likely. However re-infections can occur even when the root canal is done ideally. Recurrent decay (a new cavity under the final restoration) can get into the sealed canal space and cause a re-infection.
Sealing with Gutta Percha This is an excellent opportunity to talk about root canals. A root canal (or Endodontic [endo = inside, dontic = tooth] treatment) is performed when the pulp chamber inside a tooth becomes infected. The pulp chamber is the hollow area inside a tooth that houses the nerve and blood vessels. The nerve and blood vessels enter the tooth through a very small hole at the base of the root (see image at the very top of this page). The most common reason for infection of the pulp is bacterial contamination due to decay, a cavity gets deep enough that it penetrates the pulp. Once the pulp is infected, the immune system cannot bring enough blood flow through the small portal at the base of the tooth to supply an adequate immune response to heal the infection. The tooth must either be extracted or the all the nerve and vascular tissue must be removed from the pulp space. Removal of the tissue within the pulp space, sterilization, and subsequent sealing of the canal space is what a root canal consists of. A root canal begins by removing all decay and providing a clear access hole to the pulp chamber and canals. The canals are then cleaned and shaped using small files. Cleansing refers to removal of all bacteria, nerve and vascular tissue. Shaping refers to widening the canals to remove potentially infected tooth structure and allow adequate room for the filling material. During the cleansing and shaping process the canals are rinsed and sanitized using a diluted bleach solution (all of this is done with a rubber dam to prevent the bleach solution from entering the mouth). Once the cleansing and shaping of the canal is completed the canal is dried and filled with a thermoplastic (softens when heated) material called gutta percha. The material is heated to soften it and it is condensed into the canals so that is fills in all the space, sealing cement is also used to further assure all spaces are filled and sealed. The root canal is now finished and a permanent restoration is needed to fill in the space created by the decay and access cavity. Root canal treated teeth often require a crown to help prevent fracture. Root canal treated teeth have a much higher risk for fracture because they have often lost a considerable amount of tooth structure due to decay and the access cavity. A root canal can become re-infected for a variety of reasons. If the canal space is not cleaned out thoroughly or if it is not adequately sealed a re-infection is more likely. However re-infections can occur even when the root canal is done ideally. Recurrent decay (a new cavity under the final restoration) can get into the sealed canal space and cause a re-infection.
2010-07-05 19:53:23 Do any dentists in Yolo County or nearby counties use rectangular collimation? The recommendation to use it has been in place since 1989 because it reduces x-ray exposure to 1/4 of what it is with round collimation—and it makes a sharper image by reducing scatter radiation. Do dentists fear the small increase in reshoots more than they fear over-radiating their patients by a factor of four? While it is wonderful that most dentists now use ultra-fast F speed film or digital receptors to help reduce radiation exposure, ADA and others say to use both the fast receptor and the rectangular collimator. Why is this taking so long? Thank you. —BarbaraKing A collimator is the “cone” or cylinder that attaches to an x-ray unit. A collimator directs the x-ray beam. Using a rectangular collimator can reduce the amount of scatter radiation but it also increases the amount of “cone cuts” or operator errors that require retakes. Round collimators are used in most dental offices to reduce the need to retake films. I am not aware of any offices that use rectangular collimation in Davis or Yolo county. I think the reason most offices have not switched is because retakes can be a significant burden, and given the very low radiation exposure of current dental films the need to further reduce exposure is not viewed as a critical issue. —DagonJones
2010-07-12 10:37:43 This is a question I was asked recently and I thought I would post it here. A patient wanted to know if brushing after every meal (about 5 times a day) can cause harm to the enamel of the teeth.
Yes, brushing after every meal can harm your teeth but it is not likely to cause too much damage. When you eat acidic or foods high in carbohydrates an acidic environment is created in your mouth. This acidic environment temporarily softens the enamel of your teeth (the enamel will re absorb minerals and harden in about an hour). If you brush immediately after a meal you can remove some of the softened enamel. I recommend brushing 2-3 times a day and generally before meals or at least 60 minutes after a meal are best. Brushing more than 2-3 times a day does very little to remove additional plaque and does not have much effect on your risk of developing cavities.
2010-07-20 16:43:03 Hi! Thank you for your page. I am an international student at UCDavis and one of the worst things for a foreigner is to learn how to deal with health related issues. Things are done differently in every country, so I guess that helping us to understand dentist procedures could be a nice addition to your page. If interested, I have two questions right away. First, is it common that your main dentist does not pull teeth? In my country that is one of the most basic things but here, I was referred to another dentist who took a whole new set of Xrays and photos and even had his hygienist explain to me how to brush my teeth (which had already been done at my main dentist's office). Of course that was charged and with that visit (plus my main dentist one) I maxed out my insurance. I do not know if that is poor coordination btw the offices or standard practice. Ah, and the second one did not even pull my tooth so I am flying to my country to have the extraction done. Second, if I wanted to change my main dentist, would the new dentist accept the x rays that I already have taken? I don't feel comfortable with Xrays exposition when unnecessary. And how do I know if the new dentist would perform extractions? Thanks! —CarlaGomez
In California it is rather common for general dentists to refer all extractions to an oral surgeon. However, many general dentists (myself included) have a lot of experience with extractions and do perform them in their office. It is just a personal decision by the dentist. You have a legal right to get a copy of your x-rays (your dentist may charge a duplication fee), your new dentist will likely accept the films you bring in as long as the quality is good enough to perform a thorough diagnosis. If you want to know if your new dentist performs extractions just ask the receptionist when you call to schedule an appointment. Good luck! —DagonJones
2010-07-28 11:52:27 When a tooth is extracted, has it become standard practice to pack the empty socket with graft material, whether or not implantology is contemplated?
I ask this because this is what was told me by an oral surgeon. He stated that the bone should be restored for the benefit of those teeth adjacent to the extraction site. My insurance company does not cover this part of the procedure; however, if the application of bone graft material is now considered standard, then I should challenge their denial of coverage.
What is your opinion?
- - Herb
It really depends upon the situation. Placing bone grafting material into a socket (aka socket preservation) is a very good idea if there has been destruction of bone due to gum disease (periodontal defect) or infection from the tooth that was extracted. However, socket preservation is not always needed, there are many situations where bone grafting is not going to do much at all. Socket preservation primarily helps maintain the buccal to lingual width (that is cheak to tongue distance) of the bone ridge. Preserving this width does not do much to help maintain the integrity of the neighboring teeth but it is good to preserve natural looking gum tissue in visible areas of the mouth, especially when a replacement tooth (implant or bridge) is planned in the future. So to answer your question more directly, I do not feel like socket preservation is the standard of care in all situations, but for some situations it is a very good idea. If there is extensive bone loss very close to the adjacent teeth due to periodontal disease or infection, then socket preservation will be a benefit for those teeth. Let me know if you have more questions—DagonJones
2010-08-05 16:14:57 hi dr. jones, my dentist told me (based off of diagnodent) that my wisdom tooth has a cavity on it (a number around 38). she wants to extract it. would it be possible for a regular filling to go on my wisdom tooth instead of an extraction? could that be done? —lifeatapoint
2010-08-05 16:17:45 hi dr jones, another question: is it normal for a white filling right next to a silver filling (on the same tooth) and will that new white filling lead the silver filling in that tooth to expand and/or crack the tooth? —lifeatapoint
Yes, a filling can be done on a wisdom tooth instead of an extraction. You may need to have a silver amalgam filling on that tooth because the tooth must be kept dry in order to use a white filling and that is sometimes very difficult on a wisdom tooth. There may be other reasons your dentist is recommending an extraction (such as risk for gum infections around the tooth) so you should ask her about it. To answer your other question; it is fine to have a composite (white) filling right next to an amalgam (silver filling) on the same tooth. The two fillings right next to each other will not put the tooth at any additional risk for fracture. —DagonJones
2010-09-27 10:37:46 Hello Dr. Jones, What is your procedure for silver filling removal? Do you follow the guidelines listed by the IAOMT for safe removal? —lifeatapoint
For amalgam removal I usually use a rubber dam, high volume suction, water cooling, and sometimes saliva ejector under the rubber dam. According to the ADA it is unethical (and therefore illegal) to recommend to your patients that removing their amalgam fillings will have any health benefits. This has been established to protect consumers from unnecessary dental treatment. There is currently no scientific evidence that shows dental amalgam has any negative health consequences . However, I have patients who have requested I remove their amalgam fillings because of perceived health concerns. I will discuss the current scientific consensus (that amalgam fillings are not harmful) with the patient as well as possible negative consequences of using an alternative material to replace the fillings. If they still want them replaced I will do so. In these situations I take care to use a well isolated rubber dam and lots of high volume suction to remove all amalgam particles.
Amalgam, fluoride and child immunizations continue to be highly debated topics despite the consensus of scientific research that shows their safety and benefits. I believe it is a patient’s personal choice about what materials they use. I have a policy of not debating or attempting to change anyone’s mind, but I will share my opinions and clinical judgment if asked. —DagonJones
2010-11-03 19:00:48 Dr Jones—I'm curious. Having read your Xylitol info, what is your opinion of Zellies and its alleged positive effect on dental health? —PeterBoulay
Zellies look like a good product. They are very comparable to Epic mints and gums, they both have the same amount of xylitol per mint and gum. The shape and size of the gum and mints are almost identical they are probably manufactured by the same company and just branded differently. All the claims they make on their website about the dental health benefits of xylitol are accurate and supported by current research articles. —DagonJones
2011-01-24 08:27:29 Nicely done page. On root canals, you might mention that in addition to abscesses, cracked teeth can also require them. Most older folks like myself have had more root canals from cracks than infections.
I'd also appreciate some mention of emergency dental treatment. I assumed that if you were in pain and required treatment, a dentist would find a way to accommodate you. Having been in that situation with one of the most highly regarded dentists in Davis, I've found that it is not necessarily the case. Friends have had the same experience with other highly regarded dentists. Perhaps you could offer guidelines for appropriate dental emergencies and accepted medical ethics that would require that a dentist provide emergency treatment. —JimStewart
You are right Jim, sometimes fractures can go into the nerve and cause the need for a root canal. In my experience I have found that when fractures are that deep, the tooth is often not restorable because the fracture goes too far down the root. So you were lucky to be able to save your tooth with a root canal. Regarding emergencies, I am sorry to hear that you had experiences where you were in pain and your dentist was not available. Most dental emergencies can be managed with pain medication and/or antibiotics for a few days before treatment is needed, so often during a weekend or after hours all that is needed is to phone in a prescription. If there is trauma or other significant issues that require immediate attention Dr. Johnson and I will see patients in the office during off hours. Most dentists I know have an answering service or a cellphone that they use to let patients get in touch with them after hours. If we go out of town for the weekend we make sure that there is another dentist who has agreed to take any emergency calls for us while we are unavailable. The practices I just mentioned are pretty standard for the dental profession. Unfortunately not all dentists are as diligent about keeping their phone with them or being as available as they should, and sometimes patients think they need to be seen immediately when the issue is not necessarily as urgent as they might think. Hope that addresses the issues you were interested in. I can come back later and add some detailed information about what types of emergencies require immediate treatment and which ones can wait a few days. —DagonJones
Dental Emergencies
Fractured tooth: Most fractured teeth are on back teeth that have old amalgam (silver) fillings. Most fractures result in a cusp and/or part of the filling falling out. Sometimes there is sensitivity to cold and heat or no symptoms at all. In these situations it is not necessary to see a dentist immediately. The exposed tooth structure will need a filling or crown but will not be further damaged by being exposed for a few days, after several months the area may start to decay due to plaque accumulation. Sometimes part of the tooth that broke is still attached to the gum tissue. Part of the tooth wiggles and wobbles (and is often rather painful) but wont come out. These situations often require treatment within 0-48 hours because the fractured portion must be removed under local anesthetic (it is just too painful otherwise). If there is intense pain that is present all the time on a fracture tooth then urgent attention is required. If there is bleeding from the inside of the tooth that means the nerve is exposed and the tooth will need a root canal or extraction.
Tooth knocked out or loose: in these situations urgent care is needed. If a tooth is visibly loose and there is bleeding from the gums around the tooth the tooth will need to be repositioned and stabilized by a dentist ASAP. If a tooth is knocked out completely, gently rinse off any debris from the tooth in water and take care not to touch the root. Store the tooth in milk or in the mouth of the patient (but try not to swallow it) and contact a dentist ASAP. In some situations the tooth can be re implanted but the success rate is low. If the tooth that was knocked out is a baby tooth then re implantation is not recommended but urgent care is often needed to address other teeth that may be loose or damage to the surrounding soft tissues.
Toothache: Most toothaches do not require urgent care. Most dental pain increases slowly and can be managed with prescription pain medication and/or antibiotics until regular office hours. Antibiotics are only needed if there is swelling (size of a marble or bigger swelling). Sometimes dental pain comes on strong and fast, if the pain is very severe then urgent care may be needed.
Please post on this page if you think of a common dental emergency that is not described above.
2011-01-31 12:26:00 I've had a crown for several years, and in the last few months I get random pain now and then, usually lasting from 10 minutes to an hour or two. Due to general sensitivity (especially to cold) I use Sensodyne toothpaste. Talked with my dentist about it, and she said it looks like I stress-grind, and the grinding pressure on top of the crown is what gives me the pain. She said the fact that I don't feel the pain everyday but rather every few weeks is an indication of that. Anything, other than a mouthguard (or yoga/massages for stress :P), that I can do? —EdWins
There are many things that can cause biting sensitivity, and one of them is frequent clenching or grinding. A membrane of ligaments surrounds the area between the root and the bone. These ligaments can become irritated from too much force and can cause sensitivity in the tooth. Sensodyne is not likely to make a difference for this type of sensitivity, that only really works for sensitivity to cold/heat. A nightguard usually works best, you should also have your dentist check the bite on the crown (she probably did this when you mentioned it), if the bite is a little high an adjustment might reduce the discomfort. What you are describing is very common, even on teeth with no previous dental work. The good news is that the discomfort is often minor and temporary. —DagonJones
2011-02-01 12:45:48 Last year during an overzealous routine clean, about half of one of my top molars broke off horizontally. My dentist reconstructed the tooth, but six months later it broke off again. Now he says I must have a root canal and crown, because he says he has no idea if the root is damaged; there is quite a bit of the tooth left, and it is not discoloured or sensitive. Being terrified of dental work (traumatized as a child), I really don't want to go the root canal way. As this seems to be a purely preventative measure, is there another option apart from extraction. The dentin is exposed, but I'm wondering whether the remaining part of the tooth could be sealed or capped in some way to protect it from decay or infection. I'd appreciate a second opinion. —MaryKeast
A root canal is sometimes needed (even when there is no damage to the nerve) in order to place a post and core to support a crown
I won't call what I am telling you a true second opinion because I have no way of knowing the details of the situation without doing an exam. Having said that, sometimes a root canal is needed to place posts into the root so that the posts can help retain a buildup that is needed to help support a crown. However, that does not sound like the situation in your case. You may have the option of doing another filling (which will likely break off again as the first one did), or a crown. It sounds like a crown is going to be WAY better than another filling. You could have a crown without a root canal first. Lets say you get the crown and no root canal, and a few months or years later it becomes apparent the tooth did need a root canal. A root canal can be be performed by drilling a hole through the chewing surface of the crown. As long as the crown is gold or porcelain fused to metal (and not a full porcelain crown) then it is very unlikely the crown will need to be replaced to do the root canal. It is always preferable to do a root canal before a crown because the alternative damages the crown, but it is rarely necessary. —DagonJones
2011-03-07 19:41:04 Hi, I had leukemia treatment 13 years ago which has resulted (amongst other things) in my having a permanent dry mouth condition. I've had a multitude of cavities because of this, and during a recent half year of extreme stress, I developed significant periodontal disease. I had non-surgical treatment for it, and my dentist told me last month that I no longer have any gum pockets and very little plaque(hooray!). Since the three-month long periodontal disease treatment (ouch!), I have been maintaining my teeth with a 35-40 minute session every night, in which I floss, brush with inter-dental brushes, and use a high-quality electric toothbrush for 16-20 minutes. My question is, am I brushing too much? I am under the impression that I do not have any enamel left (is that possible?), but I am very worried about keeping my own teeth (I'm only 33). Is my tooth routine too extreme? —AmberWilkin
First off it is great that you are keeping such a diligent oral hygiene routine, that will really help you to prevent the progression of periodontal disease and decay. However, it does sound like you are overdoing it. You really should not need to brush longer than 3 minutes to get every area as clean as possible, flossing and inter-dental brushes should take about another 1-3 minutes. If you are using a soft bristled toothbrush (like a sonicare) it is unlikely you will do any damage to your teeth from over brushing, damage can occur if you are being very heavy handed or using a very abrasive toothpaste (such as one with baking soda). It would be very hard to brush off all the enamel on your teeth (so don't worry about that). But I would recommend reducing your brushing time. Talk to your hygienist next time you are in for a cleaning and show him/her your technique. Please let me know if you have any other questions. —DagonJones
2011-04-15 13:35:30 I don't live in Davis so hope it's. OK to post (although moving very there is tempting!) My question is - I had a root canal in 7 from a car accident but for some reason there was an unresolved fracture. Later my tooth broke at fracture and needed a post and crown - another dentist did that work and I left the temp on for quite a while with no problems. Finally got the perm crown and now experiencing excess saliva, which is doubly odd because I had dry mouth before due to medications. It's been about a month. Is this just an adjustment period or should I be concerned? The new crown fits a little differently (better) than the temp but they did make it thicker on the back (I think because my original tooth was thin). Thanks for your mouth. At first I was glad my mouth wasn't dry but it's gone way too extreme. —EmmaInteresting
It is certainly ok to post here if you don't live in Davis (even if you had to live in Davis to post there is no way to confirm that so I don't really care.) I have never heard of a crown causing excess saliva. I don't see how it would be possible unless you were playing with the crown a lot with your tongue. The excess movement might stimulate some more saliva flow but I doubt it would be noticeable. If you stopped using certain medications around the same time, you might be perceiving your now normal saliva flow as excess considering the change. Excess saliva flow will not cause any problems for your teeth or gums, in fact it will help prevent cavities (saliva naturally fights decay). —DagonJones
2011-06-03 13:37:15 Hey Dr. Jones, you are taking my wisdom teeth out in a couple weeks, but I figured I would post my questions here so everybody could benefit from the answers (plus I'll hopefully be too doped up on the day to remember anything, let alone have a coherent conversation).
I've already made a list of soft foods to eat after the surgery (pudding, mashed potatoes, applesauce, plain yogurt, soups, cream of wheat, refried beans, etc. if anybody needs ideas) and I've heard the typical advice about not using a straw, not eating anything hotter than lukewarm, that kind of thing - but I was wondering about some gray areas:
Peanut butter: too sticky? Pureed Indian food: too spicy? (also, if I get my "supremely spicy" flavor hummus is that bad?) I also heard that drinking pineapple juice and biting down on black tea bags will speed the healing process. Old wives' tales?
Thanks and see you soon! —MeggoWaffle
- If it's anything like when my wife had hers out (not by Dr. Jones), find somebody you really trust and who is competent to take care of you for the rest of the day. You'll need mental as well as physical support: coming out of anesthesia will have you asking for the wrong things (like asking to call people over and over again before you can even be understood because you keep forgetting you've already asked), so you need somebody who can think on your behalf and be patient as you come back to your normal self. I'll leave the food and other technical stuff to Dr. Jones — and maybe you're not going to have the same kind of anesthesia, but if you do need somebody "to observe you", start thinking about who you trust to be patient and understanding for several hours with you. Best of luck — may you heal quickly and get back to unblended Indian food as fast as possible. 8Đ ⁓ʝ⍵
Peanut butter is just fine. Indian food might be a bit spicy and therefore irritate the extraction sites but if it does not hurt while you are eating it then you should be fine (just make sure you eat only bland foods if you are still numb). Pretty much any food that is comfortable to eat is ok. Black tea bags contain tannin which constricts the blood vessels and reduces bleeding but will not speed up healing. Pineapple juice does not seem to do anything special, I found several references to it reducing swelling or helping healing on a Google search, but nothing from reputable sources. I searched for research papers on this subject and found nothing so it is most likely an old wives tale. In regards to the anesthesia, you will be rather sleepy and out of it for several hours afterwards so it does help to have a "babysitter". We will not be using general anesthesia or IV sedation so your sedation level will be rather light and easier to come down from. —DagonJones Update on Pineapple Juice: It has the chemical Bromelain in it, which supposedly reduces swelling. There is a German study from 1989 that found that it reduced swelling a small amount following third molar extraction, but not enough to be statistically significant. So I still don't think it will do any good. On a side note Grapefruit Juice can increase the effect of many medications because it inhibits an enzyme called Cytochrome P450 (CYP450). This enzyme is responsible for breaking down many medications in the blood stream. So if you have less of the enzyme, the effect of the medication is increased. This is generally undesirable and can cause dangerous difficulties with breathing if taken while using sedatives or anesthesia so it should be avoided when taking any medication.
- That's good to know because I actually love grapefruit. Thanks for all the other info too, see you next week! -Megan
2011-10-02 20:18:04 My 14 y/o daughter has a 12 yr molar that the dentist says x-rays show adult tooth coming in crooked has only eaten away one root. Dentist planned to sedate and remove the tooth which I would have to pay a co-pay for. I told her I'd pay her if she could remove it. She did. I am worried now if she left any root in, have we created a worse problem? Or will her body just reabsorb it as the adult tooth pushes up. Thank you for considering my question. —DebbiJohns
Good question, however, I am a little confused. The 12 year molar (aka 2nd molar) is an adult tooth that erupts into the gums behind the first molar without replacing a baby tooth. I am assuming that she had a baby tooth removed to make way for the adult tooth. It sounds like the adult tooth did not resorb (eat away) all of the roots of the baby tooth, and therefore the baby tooth would not fall out on its own. If the baby tooth was extracted and a portion of root was left behind, most of the time the remaining root will be resorbed or remain in the bone without any problem. In rare situations the root can become infected and require further treatment. Check the area every few days, if the area is very red and swollen and your daughter reports increasing pain, that would be a sign of infection and she needs to go back to the dentist soon. Even without any infection the area should be monitored every 6 months to make sure the adult tooth is erupting normally. Please let me know if you have any other questions (or if I was wrong in my assumption). —DagonJones
2011-12-08 17:54:44 Hi Dagon I was asking a friend of mine a dental question and I was referred here: I had a filling fall out a while back and it is now really starting to hurt me, how much do you think it would cost to get repaired? I didn't realize it had fallen out until now it is located in the top right middle side of my mouth. Thanks —KellenRuel
When I had the same thing happen, I went back to the same dentist that did the filling in the first place and he redid it for free. —TomGarberson
Tom brings up a good point. Most dentists will replace a filling at no charge if it was done within a year or two, of course this depends on the circumstances of the situation and the individual policy of the dentist. If the filling just needs to be replaced it could cost anywhere from $150-$250 depending on the size of the filling and the type of material used. The fact that you are having pain is a concern because this indicates there is likely decay on the tooth and it may have entered the nerve. If that is the case the tooth will likely need a root canal and a crown (see the above description about root canals "here"). If the tooth needs a root canal and crown there is considerable more work involved and the fees could be $1300-$2000 depending on the tooth. If you have dental insurance, your insurance will cover a portion of the fees. If the tooth is hurting all by itself (it throbs or aches when you are not touching it or eating) then that is a sign it will likely need a root canal. If it is just sensitive when you drink cold liquids and the pain goes away immediately after the cold is gone then that is a normal reaction for a tooth that has lost a filling and you most likely don't need a root canal. It sounds like the filling fell out and it felt fine for a while but now it is hurting, this is most likely a situation where decay is present and it has spread to the nerve and you will probably need a root canal or extraction of the tooth. I would advise you to see a dentist soon because you could develop an abscess in this area which is often very painful and a significant infection which will need attention. I hope this helps and I wish you good luck. —DagonJones
2012-01-04 05:42:59 Hi Dr. Jones, I was a regular seeing my dentist twice a year but getting 4 cleanings per year. At my March visit the Hygenist was very aggrssive and scrapped hard and hit my teeth with the polisher and pressed with Her weight against fronts and back of teeth. I was in a state of shock and asked what she did and she said it was just the polish that I was seeing. Lumping as I was rinsing. My tongue on the back of the 4 bottom front teeth felt strange like they were too clean. After that food started sticking too my teeth and food did not taste right. Choking on food as I tried to eat. Now all my teeth are yellowing some translucent, you can see verticle cracks and the sensitivity is constant. I had no sensitivity until this cleaning. I had amalgram fillings from a young teenager and they Are all raised and blackened. Saw dentist in June and begged him to fix 1 molar with a crown as it was raised so high and exposed on the whole tooth. He said he wanted to wait. I went back the following month and he said my teeth are to thin and they all would need to be capped. The 8 bicuspids that never had any fillings are all worn away. I told my spouse about this as I went regular to dentist and to have this happen All at once and not over a period of time seems odd. I note he fired the Hygenist I had for all those years. When we went for the consult he said we will cap them when I deem it necessary. I felt it was necessary then. Nevertheless, he let me suffer and I went to another dentist that said all my fillings were cracked and he worked on upper left and bottom right and now my bite is off having headaches difficulty eating and speaking. My face is distorted, mouth difficult to open, air hurts all the teeth I have hard calculus forming 2 days after a cleaning, gums are receding and I am in agony. Face nose and cheek pain. Lips constantly cracking and mouth ulcers inside on gums. What type of dentist do I need? Who can determine if I have bone loss. Glands under jaw inflamed. Face sinking and redness in nose and cheek and chin area. I stopped using soma care toothbrush for oral b ultra soft. Was always a great flosser but from her scraping the floss gets stuck in every tooth and breaks off. Brushing is painful and food is getting stuck up above my teeth in my cheeks. Using biotine for dry mouth. Lips are enlarged and while all my face is shrinking they are protruding from my teeth shifting forward. Also top molars are shifting out to cheeks and bottom are going inward not the u shape they were. I have vision problems and headaches that I believe Are a result of this. If you need more information please do not hesitate to ask. I tried to have mercury Poisioning test done but not enough lipos in my blood.
I need to start by saying that unfortunately I don’t think I can be much help for you. You describe a lot of symptoms here that I consider to be out of the scope of my practice as a dentist. You list headaches, vision problems, pain in nose and cheeks, and changes to your facial structure. These are all symptoms that I do not feel comfortable diagnosing or treating. Regarding the sensitivity you are feeling on your teeth, it sounds like you have had a history of periodontal disease as this often requires cleanings 3-4 times a year. Periodontal disease can result in recession that exposes the sensitive roots of the teeth. Sensitivity protection toothpastes (like Sensodyne) can sometimes help or a dentist dispensed product called “MI paste” can be applied to your root surfaces by you at home and that often helps with sensitivity. It is common for sensitivity on root surfaces to increase right after a cleaning because tartar is removed from the surface of the roots. This tartar should be removed because it contains lots of bacteria that can make periodontitis worse, but it also covers the sensitive surfaces of the roots and removing it can increase sensitivity. Regarding the vertical fracture lines in your teeth; under the right lighting you can often see dozens of small cracks in the enamel of teeth, these are called “craze lines”. They are confined only to the enamel, cause no pain, and are very common. No treatment is recommended for craze lines You also mentioned your bite is off after some recent dental work. This could be a result of some of the fillings being too high, they may need to be adjusted. I would suggest having the dentist who placed them check for high spots. Often when multiple fillings are done it may be impossible to get the exact same bite as before, this is not always a problem as many people will adjust to a slightly different bite within a few weeks. Regarding the shredding of floss between your teeth, this is often caused by very tight contacts between teeth or very rough fillings. Aggressive scaling of your teeth by a hygienist would not be able to tighten the contacts, and often would result in smoother surfaces of the fillings unless a filling broke or chipped during the cleaning. I do not think the flossing difficulties are a result of the cleaning you described. I would recommend a high quality floss like Glide. High quality flosses slide easily between tight teeth and tend to shred less. You also mention food sticking to your teeth, food not tasting right, choking on food while eating. I am sorry to say that I do not know what could be causing these symptoms. I cannot think of any reason why they would be caused by a very aggressive cleaning. I am very sorry to hear you are in so much discomfort and I understand you are very concerned about all the changes you described. I would strongly suggest that you start by seeing your physician to discuss the headaches, facial pain/redness, and vision problems. These could be symptoms related to a systemic heath problem. If you have any other questions please feel free to ask and I will answer to the best of my ability. —DagonJones
2012-01-04 11:30:59 Dr Dagon: Can you please provide your opinion on using amalgam for fillings? What are the alternatives to amalgam and do they last as long? —BrianPaddock
Dental Filling Materials
Here is a link to the Dental materials fact sheet that is required to be provided to all patients by the Dental board of CA. This is a very nice pamphlet that details the strengths, weaknesses, and toxicity concerns of available dental materials. I consider amalgam to be a safe, good restorative material. There are situations when amalgam is the best material. Each material has its own strengths and weaknesses. Amalgam is not a pretty color, but it works well in a moist environment and does not require enamel to bond to the way that composite (white fillings) do so it can be used when composite should not be used. It is less technique sensitive than other materials so it usually lasts longer when used in difficult areas to access (like behind the last molars, or on people with very limited opening). It is very durable to compression forces when it is at least 1.5mm thick, so it is a very good material for medium to large fillings. It typically lasts longer (but not necessarily) than composites because it is less technique sensitive, conditions have to be just right to get a long lasting composite filling. Amalgam is not the best material for very small fillings because it requires a certain thickness to be strong. The most common alternative to Amalgam is Composite. Composite is a resin (basically a plastic) reinforced with particles of silica. Composite bonds very reliably to Enamel (the hard outer layer of teeth) but less reliably to dentin (the softer inner part of a tooth). For this reason it is not appropriate for cavities that are deep between the teeth because there is often a lack of sufficient enamel on the deepest part of the tooth and moisture control is difficult. Provided moisture can be controlled a composite can be used in a situation like this but it will have a higher chance or recurrent decay than a comparable amalgam filling. Compisite is very strong even when it is very thin, for this reason it is better than amalgam for shallow, conservative fillings. Another family of tooth colored filling materials are Glass Ionomers and Resin modified Glass ionomers. This family of restorative materials bond to the tooth via a chemical reaction. They absorb and release fluoride over time so they are very good at resisting recurrent decay. They are rather weak to compressive forces and therefore are not appropriate for the chewing surfaces of adult molars. They work well in a moist environment so they a good alternative when moisture control is difficult. Glass ionomers work best for cavities near the gumline. If someone has a deep cavity that involves a chewing surface in a back molar and does not want an amalgam filling, using only a glass ionomer would not be appropriate because it will not withstand the compressive forces over time. So sometimes Glass ionomer and composites can be layered to provide a good long lasting alternative to Amalgams. This technique (sometimes called a “sandwich” technique) contains multiple steps. Due to this fact it is rather technique sensitive and time consuming, so there are more potential for problems like voids between the filling layers. Other restorative materials include laboratory made gold and porcelain restorations (crowns, inlays and onlays). These restorations have to be made in a lab from an impression of the prepared tooth. Due to this fact they often require 2 visits (but may not if the dentist has an in house computer aided milling machine). Due to the additional expense and time involved these restorations are more expensive than a direct placed filling material. Laboratory made restorations work best when there is extensive destruction to a tooth or fracture of the tooth is a concern. Direct filling materials (amalgam and composites) can leave a tooth susceptible to fracture, especially when the filling is very large. Most gold and porcelain restorations are designed to cover the cusps of the tooth and therefore help prevent future fractures. I was taught and personally think gold is the best restorative material for medium to large restorations. The margins (the area where the restoration meets the tooth) of gold restorations are often smoother than porcelain therefore resulting in less plaque accumulation. There is a lot of information and detail I can go into about each material but this provides a pretty good overview. If anyone has further questions please follow the link to the dental materials fact sheet or feel free to ask. —DagonJones
Gum Grafts
 The junction between hard gums and thin mucosa
The junction between hard gums and thin mucosa 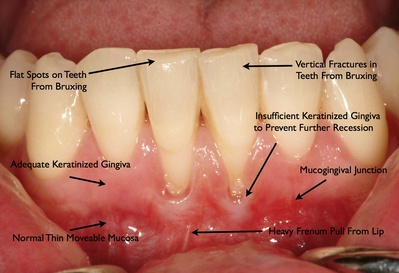 Recession on two central incisors There are two major reasons a patient is referred to a periodontist for an evaluation for gum grafting. First and most important is to stop recession and bone loss around teeth to prevent the loss of that tooth (or teeth). Second and less frequent is for repair of esthetic defects. Many times, after treating a tooth with a gum graft to restore health and prevent further recession, the tooth also looks better esthetically because the exposed root has at least been partially covered with the gum graft and has less recession.
Recession on two central incisors There are two major reasons a patient is referred to a periodontist for an evaluation for gum grafting. First and most important is to stop recession and bone loss around teeth to prevent the loss of that tooth (or teeth). Second and less frequent is for repair of esthetic defects. Many times, after treating a tooth with a gum graft to restore health and prevent further recession, the tooth also looks better esthetically because the exposed root has at least been partially covered with the gum graft and has less recession.
What happens when a patient is referred for an evaluation of gum recession? I will address that issue and any factors that may contribute to the gum recession including the lack of sufficient hard gum tissue around the tooth. The are two basic types of oral tissues in the mouth: keratinized non-movable hard tissue around the teeth for protection during chewing and mucosa which is more thin and delicate but movable. These tissues have very different functions which is evidenced by their macroscopic and microscopic anatomy. If there is not enough hard keratinized gum tissue around the tooth then there can be progressive loss of gum tissue and bone. Genetics is probably the biggest factor contributing to recession. People with fair delicate skin generally have fair delicate gum tissue that is more susceptible to gum recession because their gum tissue is traumatized and torn easier during chewing or tooth brushing. Some people also have genetically strong frenums, which is the attachment from the lip. This can predispose them to recession. Another common factor is using or having used in the past a tooth brush with medium or stiff bristles. Years ago dentists used to tell patients to use stiff tooth brushes because they clean better. This is true, but we found that it comes at the cost of causing recession more often. Most dentists now recommend soft or extra-soft tooth brushes. Soft tooth brushes might not clean quite as well, but they are safer for the gums. Likewise, if a patient is using a very abrasive toothpaste (especially ones that advertise their tooth-whitening ability), then beware of their being very abrasive and wearing away the gum tissue. Fortunately the American Dental Association tests toothpastes for effectiveness and safety. If a toothpaste has the ADA Seal of Approval, then it is effective and also safe to use with regard to abrasiveness. A fourth factor contributing to gum recession is the tooth being out of alignment even a slight amount and being traumatized and loosened because of the way the teeth hit. In that case having their general dentist make the patient a night guard can help significantly. Another factor can be orthodontic movement of teeth. Fortunately, the orthodontists in our area are very proactive in sending patients for an evaluation before or during orthodontic treatment if they suspect a problem. Severe cases of recession usually have more than one of these factors going on simultaneously.
So why should you worry? One reason is that besides loosing gum tissue you are also loosing the bone that supports the teeth. I emphasize bone loss because where you can see the root of a tooth not only gum tissue has been lost, but also the bone that was also covering the root. The tooth is normally embedded in bone and the gum tissue covers the bone. There is an old saying in periodontics that is corny, but summarizes the problem: “The (gum) tissue is the issue, but the bone sets the tone.” Another problem is that roots are very soft, unlike enamel, and are more prone to cavities if exposed to the oral environment. When tooth roots get cavities, the decay can destroy teeth rapidly. If there is bone loss between the teeth (chronic adult periodontitis) in addition to bone loss from recession on the outside surfaces of the teeth, then the situation is more complicated.
What can or should be done? The generally accepted treatment for progressive recession of gum tissue (along with the bone loss that accompanies recession) due to the lack of sufficient hard gum tissue is the addition of hard gum tissue by a gum graft. I emphasize the word progressive because not all recession needs to be treated with grafting. If someone has been using a stiff tooth brush and has lost some keratinized gum tissue around their teeth but still has enough keratinized tissue remaining to resist further recession, then the treatment of choice may be to simply switch the patient to a softer tooth brush and monitor for further recession. This will many times prevent further recession and bone loss. If there is not adequate hard gum tissue to prevent further recession then a gum graft should be considered. The gum graft (a general term which includes “free gingival grafts”, “connective tissue grafts”, and “pedicle grafts”) has more than 50 years of clinical research and there have been many thousands of research publications over the years in refereed scientific journals as to its effectiveness. The gum tissue that is grafted can come from the roof of the mouth or from a tissue bank. The autogenous tissue (from the roof of your mouth) is firmer and harder than the allogenic tissue (from tissue banks). But using the tissue from tissue banks eliminates a second sore area. The area on the roof of the mouth usually feels like a pizza burn for a week or two, but will totally fill with new tissue in within a few months.
What are the side effects and contraindications? The main side effect is soreness on the roof of the mouth. Patients should kick back for a day or two and sip cold liquids over the surgery areas. I usually give long acting local anesthesia so people can go home and place cold liquids (such as ice water) on the surgery area while still numb. Cooling the surgery area during and after treatment will reduce any bleeding, swelling or post op soreness and help things heal faster. Some people notice a temporary sensitivity to cold that goes away within a few weeks to months. Applying desensitizing agents at post op visits helps greatly. A major contraindication is if patient does not want it. Uncontrolled high blood pressure or uncontrolled diabetes are also contraindications to gum grafting. Unrealistic expectations is also a contraindication. The larger the amount of recession and the more the bone loss, the less root can be covered for esthetics. Plus, everybody heals differently. I can do the same exact procedure on two different patients and have two different results. One patient may get significant root coverage and the other minimal. Although getting root coverage is not totally predictable, getting adequate hard tissue for health and to prevent further recession is very predictable. Clear communication between the doctor and the patient is very important before starting gum grafting. It is important that the patient understands the risks, benefits and alternatives to various treatments and then makes an informed decision as to their course of treatment and accepts responsibility for their decision. —DavidJolkovsky
 Dark spot indicating bone loss and infection
Dark spot indicating bone loss and infection  A Fistula, an area where pus is draining from an infection
A Fistula, an area where pus is draining from an infection
2012-01-09 01:25:05 I am a college student on a very tight budget and have a question. I had a tooth that had decay extra deep and when the dentist drilled it out he said he might have left a microscopic hole in my tooth which would lead the a nerve. He put a special sealent on it to hope and save it. He told me if it was sensitive to hot or cold I would have to get a route canal. The only problem is I can't afford one. It hasn't became sensitive to hot or cold yet but I am wondering if it does, will not getting a route canal cause any other harm to my body besides pain? —kamogurl1213
What you are describing is a rather common situation when decay is very deep. The deepest part of decay can penetrate a very small section of the pulp chamber (nerve canal space), if this happens bacteria can enter the pulp chamber and lead to an infection that requires a root canal. This situation can also happen when the decay is very close to the pulp chamber but there is not a visible penetration into the pulp chamber. It is unpredictable to determine whether or not the tooth will need a root canal. In my opinion, your dentist did the right thing by placing a seal over the exposed area and asking you to look out for symptoms. If the tooth needs a root canal it may take months or years before you notice symptoms. You will most likely notice a throbbing pain that occurs for no reason or pain to cold that lingers for several minutes after the cold stimulus is gone. It is possible for an an infection to occur in the root (requiring a root canal) but you will have no symptoms at all. This situation can be detected by taking screening x rays of the root, a dark circle will show up on the x ray around the tip of the root indicating there is an infection present. To answer your question, if an infection develops and you do not get a root canal the infection can become severe. These infections can be (but are not often) life threatening. Usually the pain is so severe that people have to go to the dentist for either an extraction or a root canal. Pronounced facial swelling can occur due to the infection. Sometimes the infection is not very severe and if the pus can drain (usually through a small hole or "fistula" in your gums that looks like a pimple) then it may not be painful. In any situation it is best to get the root canal or extraction, if an infection is present your body is constantly fighting off the infection and bacterial toxins are created. All of this is not good for your overall health. As the infection continues bone around the tooth will be lost (this can be regenerated later). In your situation I would wait and watch for any symptoms, if the hole to the pulp chamber is small there is a very good chance the tooth will be just fine and you may not need a root canal. —DagonJones
2012-03-10 09:21:47 I am a high blood pressure patient who recently visited a dentist because of toothache. I had thought the enamel on one of my molars was slightly eroded only to find out that I had an infection in my gums. Without any prior antibiotics given, the dentist proceeded to perform a partial teeth cleaning (emphasizing the need for me to come in thereafter several times a year to have my teeth cleaned). This led to further complications as my jaw swelled up with an abcess the size of a nickel. I was in pain for several days thereafter and had to return to demand a prescription for painkillers. Is this proper procedure in cases like these? —TokunbohJiboque
"infection in your gums" most likely refers to periodontal disease. In which case cleanings several times a year are very important as well as Scaling and Root planing (deep cleaning). It is not standard to give antibiotics before a regular cleaning or Scaling and root planing. As a result of a cleaning, sometimes a localized infection and or irritation may occur. This may require antibiotics or pain medication. To answer your question it sounds like pretty standard procedure, however usually a hygienist does the cleaning not the dentist. I would recommend you get a deep cleaning (scaling and root planing) if you were diagnosed with periodontitis. —DagonJones
2012-03-16 23:56:45 I have just had 9 teeth removed and my jaw keeps slipping out of place and I've tried to use a bite guard but its causing more damage to my jaw and when I use the bite guard it hurts my jaw. I just wanted to know if there's anything you'd recommend, because surgery isn't an option, oral surgery has already caused this problem. —RaevynJasmyn Jaw issues can be very frustrating and difficult to diagnose and manage. Unfortunately in order to understand the specific issues that are happening with jaw disorders a physical exam is required so the dentist can feel what is going on with the joint. I would recommend seeing your dentist for a TMJ exam as I am unable to give any sound advice without a physical exam in this situation. —DagonJones
2012-03-31 21:51:11 Dr. Jones, I just had a gold onlay pop off while I was flossing! Of course, this has to happen over a weekend. Is it OK to wait until Monday to see a dentist? Any other activities I should avoid? (other than chewing on that side) —RobertaMIllstein
Inlays do come out from time to time. It is fine to wait a few days to get it re cemented. When an inlay or filling between the teeth is lost food is likely to get caught between the teeth. Be sure to floss or use a toothpick to get this food out after meals. —DagonJones
2012-04-13 12:27:14 What are the best ways to battle bad breath? —JenniferCook
Most bad breath odor comes from bacteria that live on top of the tongue. Try a tongue scraper as they work better than brushing the tongue, also mouthwashes tend to help by overpowering any odor with mint. —DagonJones
Fresh rosemary will get rid of garlic breath. As in, rosemary seems to actually get rid of bad breath rather than overpower it. Another way to help battle bad breath is to eat fewer sugar-sweetened things, at least in my experience. —Angel.York
Can't bad breath sometimes be the result of an underlying dental problem? —CovertProfessor
2012-05-08 10:15:13 About 15 years ago, my dentist broke a file in my tooth during a root canal. Today, I went to another dentist b/c I have a pain in my jaw below the tooth where the root canal is. The new dentist said I need to go to an endodontist and have the file extracted. My question is this. Who is responsible for paying for the file extraction? Me or the original dentist? Thanks. —JackieEldridge
I understand that this is a rather frustrating experience for you, however, file separations are a rare but often acceptable outcome. When a file breaks off the accepted method of treatment is to finish the root canal and leave the file in place as part of the filling material then monitor the tooth for symptoms or signs of infection. If 15 years went by without any problems it sounds pretty successful. Even if the file had not broken off and the root canal was done as perfect as possible you might still have a re infection of the root canal system because root canal treatments do not always last forever. It may not be the file that is causing your symptoms. So to answer your question it would be your responsibility to pay for the re treatment. Your question is actually more for a lawyer than a dentist, but if you wanted to file a claim against your previous dentist to try and get him to pay you would not have a very good case. I think you would need to show that the dentist was negligent and file breakage is an unfortunate outcome that can happen even in the hands of the most skilled dentist, but it is often not due to negligence. —DagonJones
2012-05-23 11:54:08 I have a 20 month old son who still uses a pacfier. I have heard differing opinions regarding whether or not a pacifier causes damage to a baby's teeth. What's your opinion? —jsbmeb
Sorry for the delay, I was on vacation for a few days. Pacifiers and thumb sucking can cause orthodontic movement of the anterior teeth, but they will not cause decay or other problems. This is usually not a problem unless the child is using a pacifier or sucking their thumb beyond age 4. The typical result is the front teeth push forward and out so when the child bites down there is a open gap between the upper and lower front teeth. The general recommendation (which may differ depending on who you ask) is to discontinue pacifier use at about age 2, and to discontinue thumb sucking by no later than age 4. —DagonJones
2012-06-14 10:10:12 I went to the dentist yesterday, after having not seen one in awhile. My previous dentist hurt me terribly on my last visit years ago, and it kept me from seeing another one.
I don't know dental terminology for tooth id, so please excuse that. But, here's the scenario:
The problems exist on the lower teeth, back right side. On this side, I have a tooth in the far back, then a gap where an abscessed tooth was pulled, then there is the other problem tooth, located right after the gap (tooth, gap, tooth).
Problem 1: Far back tooth on the bottom right has decay that wraps around 3 sides. The dentist said it may be non-restorable, but she would try to fill it, and would probably need a crown. She did x-ray of it, but said she wouldn't know how extensive the problem was until she drilled into it. She wants to attempt to fix it tomorrow.
The tooth is giving me no trouble, and is the only back tooth I have on that side remaining that I am able to chew with. I asked the dentist, since it was a gamble to try and fix it, why didn't I just leave it alone unless/until it gave me trouble. She said that wasn't an option, and then I would be looking at a root canal.
Problem 2: The tooth in front of the gap, the dentist says, is not restorable, as it has a large cavity on the back of it.
I do notice mild sensitivity sometimes with this tooth, but nothing bad. The dentist agreed I should probably leave this one alone until it causes me a problem. When / if I have this one pulled, it will show when I smile.
I do not have the money to go to another dentist right now. I have heard of implants, but know I don't have the finances for them at the moment.
What should I do? I am scared to death I am going to go to the dentist tomorrow, and walk out without a very important tooth, losing my ability to chew on that side.
By the way, I am not referring to a wisdom tooth. All of mine were extracted years ago.
Thank you for your advice. —kbmeador
I would agree with your dentist's advice. If there is a tooth that has very deep decay it is definitely worth trying to save it. If you just leave that tooth alone because it is not bothering you now then you pretty much guarantee that the decay will go into the nerve and will need a root canal or an extraction. If your dentist cleans out the decay and finds that the decay is very close to or a little bit into the nerve then ask her to do a "pulp cap". This is placing a small amount of medication that contains calcium and will help to heal the nerve and hopefully prevent the need for a root canal. This step will improve your chances just a bit. If the tooth needs a crown and you cant afford one you can ask for a bonded amalgam filling. This is a large metallic filling that is bonded to the tooth to help it from falling out and there is some believe this will help prevent the tooth from breaking later. A crown will be much better but a bonded amalgam will be your best bang for your buck. Don't be alarmed if this tooth is very sensitive to cold for several months. If the tooth starts to ache and the pain gets worse then that is a sign the tooth will need a root canal or an extraction. Regarding the tooth that is not restorable, if your dentist says it is not restorable and it is not bothering you now then it may be best to just watch it for now. However be cautious that sometimes infections can be present and they will not cause any symptoms, so just make sure your dentist is monitoring the area every 6 months to a year. Let me know if you have any other questions —DagonJones
2012-06-22 12:45:36 Hi.. First timer. About 11 years ago, I had 2 root canals done, same time, on my 2 molars bottom right. About 6 months ago, the crown came off the tooth furthest back and I had the remainder of the tooth and roots pulled out. The other day, I went back to the oral surgeon for an implant consult and he told me that the xray (he just took) shows an abscess below the root canal of the 2nd tooth. I am not having any problems with it, but he says he wants to do surgery, or an epicore (sp?) to remove the abscess, while he's doing the implant for the tooth next to it. Does this sound right? Is it possible to have an infection below a root canal? And, why couldn't I get rid of it with some antibiotics? The extra procedure he wants to do is costly, about $800. That's on top of the implant and eventual crown. Just wondering if its necessary, or is he trying to make a few extra bucks? Thanks. —TonyFabrizio
What he is describing is a real thing. Sometimes a root canal can fail or become re infected after many years and need retreatment or an apicoectomy. I generally recommend an endodontist (root canal specialist) evaluate the tooth for retreatment but an oral surgeon can do that too. Antibiotics will not get rid of the infection because there is likely some bacteria or necrotic nerve tissue inside the tooth that will cause reinfection despite antibiotics. DagonJones
2012-06-25 14:54:17 could you please tell me what the pain i might be feeling at the roof of my mouth is i cannot eat any kind of tabasco sauces it causes me real pain. are their open holes? —NancyCollins In your soft palette? Your hard palette? Do you have open cold sores? Do you have cuts that are reacting to the spice? How bad is this pain? Can you describe it? Daubert
If this pain is new and you have not experienced it before it is most likely caused by some type of sore,lesion, or cut on the roof of your mouth. The most likely situation is trauma, either from rough food (tortilla chips) or a burn (usually pizza). If you have ever had cold sores in the corner of your mouth then the virus that causes cold sores (herpes virus) can sit dormant in your body for years and can occasionally cause multiple pimple like sores on the roof of your mouth that can be very sensitive. This type of herpes lesion almost always occurs as 5 or more red dots on one side of the soft pallate only. All of the situations I described (herpes or trauma) are self limiting and should go away within 1-2 weeks. There is also a condition called "burning mouth syndrome" that does not have a known cause. It is characterized by a burning sensation, usually on the tongue, that comes and goes. This condition affects women more frequently than men and is also associated with other neurological pain syndromes. I am not aware of any known treatment for burning mouth syndrome, but it sounds like this is not your situation as it is often characteristically on the tongue.—DagonJones
2012-10-04 20:51:07 Is it common practice for a dentist to put fillings in children without sedating and/or numbing them beforehand? —JenniferCain What you describe is quite common. Because an injection is often very traumatic for kids it is avoided if possible. If the decay is shallow or moderate it often can be removed with no or minimal discomfort, and if the child is moderately cooperative the whole process often goes very smoothly. More extensive work will require anesthetic and possible sedation depending on how cooperative the child is. —DagonJones
2012-10-12 08:01:49 My son is 14 and nearing the end of his years in braces. earlier this year they began to close a 1 to 2 cm gap by his lateral incisors. The left side did fine but the gap on his right — when it closed up his gums got deep pockets around that tooth. So when he flosses it slides pretty far up the tooth. What is the general consensus as to treat this? should people be less aggressive sliding the floss so that ligaments can reattach or should people use a WaterPik type of instrument instead of floss? we are very diligent about cleaning so it doesn't seem to be from lack of proper dental hygiene. there is no swelling or redness or bleeding. He began using Listerine a month ago but we haven't noticed a difference. Thank you so much for your time!! I can't wait to learn why this is happening and the general consensus as to remedy it. —SusanDaniels I cant say what has caused that without taking a look. The fact that there is no swelling or redness is a good sign, he should be able to floss normally, push the floss below the gums with gentle pressure until you feel it stop. It is likely that the gum tissue is just swollen in this area due to inflammation. This is a very common situation with braces and will likely go away a few months after they are removed. He should keep the area clean by flossing and brushing well with a soft bristled toothbrush. Ultimately you should have his orthodontist take a look at the area. —DagonJones
2012-10-16 10:52:00 How strong and functional are porcelain or ceramic crowns? I broke a tooth (front) last weekend and had to get an emergency temporary made immediately. It needs to last me a few months because I need to have a repeat root canal on the tooth first. Now I am worried about the permanent restoration since everything I read states temporaries are NOT strong or durable - are permanent ones much better? Once I have the permanent crown, do you have to be careful about biting things? I don't try to open things with my teeth or bite my nails or anything like that, but I just want to make sure I will be able to eat normally without worrying about it breaking off, as my only option after that is to replace it and I can't believe how expensive it's going to be. I have never had a crowned tooth, although I do have several root canals due to trauma from a car accident about 10 years ago. My other concern besides durability and strength is color match/shape match, as I need it to look natural. My temp looks amazing, I hope the final one can be made exactly the same. —JenF
A permanent porcelain crown should be quite strong, you can eat normally but just avoid using like a tool and you should be fine. The strength of a crown can change depending on the amount of tooth structure you have under the crown, if the accident left you with very little front tooth then the crown will be more prone to breaking off. If your temporary looks great then the permanent restoration is likely to look just as good if not better. Sometimes crowns need to be sent back to the lab one or more times to make subtle changes to the shade or shape to get it just right so be aware of this possibility. —DagonJones
2012-10-26 17:18:09 Hello Dr. Jones
I had a very small filling on tooth number 3 replaced and experienced quite a bit of pain afterwards when chewing. The dentist wanted to wait and see if it the pain subsided on its own so I waited a few weeks but still experienced discomfort so she removed the first filling and did a new one (both were composite). The filling also feels very awkward with sharp edges where food gets caught when I accidentally chew on that side.
She now wants to do a crown and I am concerned since the tooth never bothered me previously.
I requested that both fillings be done without anesthetic and, while they were painful, they were not excruciating.
At present, it hurts when chewing and there is often a dull pain throughout the day.
I appreciate any advice you might have!
Thank you! —tkh777
It is quite possible that the tooth has a fracture somewhere within it and may require a crown, and this might not be apparent until after the filling preparation (at no fault of the dentist). First, I would recommend trying to have the filling replaced with Amalgam one more time before going for a crown. Sometimes changing the filling material helps resolve sensitivity to chewing. chewing sensitivity is more common with composite than with amalgam. Composite is a resin material and therefore has some flexibility, Amalgam is a rigid metal and has virtually no flexibility and is therefore less susceptible to chewing sensitivity. Additionally there is more potential for voids in a composite than an amalgam and internal voids can lead to sensitivity as well. I think you will also have less of an issue with rough edges with an amalgam due to the fact that amalgam cures slowly and therefore less rough edges are created during placement and finishing/polishing. —DagonJones
On a side note recently during an infection control class the instructor informed us that the number one complaint in dental offices is assistants or doctors going into drawers to get clean equipment with gloved hands. I thought about this and realized that often a patient is sitting in the chair and can not see what is going on. We often will retrieve items from drawers without removing gloves, we use a clean pair of tweezers to open the drawer and retrieve the item, that way our gloved hand never touches any items, just the clean pair of tweezers.
2012-10-30 15:59:17 I have a question regarding my mouth.. i had a gum graph done 8 months ago but my problem is dat i have a metal piece hanging from my mouth is dat a good thing —msliline09
I'm not sure what you are talking about here but if there is a metal piece hanging from your mouth dat is probably not a good thing. It might be a suture (stitch) that needs to be removed. Call the doctor who placed the graft and describe the situation. —DagonJones
2012-10-31 17:13:52 Thank you for your quick response in regards to my tooth issue!
I have several more questions. Is there any danger in waiting to do a crown and trying to chew with only the non affected side? Since it hurts so bad, I would imagine that it is not good for the tooth when I accidentally chew on the affected side and that if it is indeed cracked, the crack is widening with chewing.
Also, the filling is towards the front of my mouth. Could I get an amalgram and composite mix for aesthetics?
Lastly, why would it not have hurt prior to the first filling. Is it more likely that the tooth was always cracked or do these things usually happen during drilling to prepare for a filling? I can't understand why it had no problems before and is now painful. How large of a crack will cause sensitivity? And should it feel similar to having a tooth drilled but less severe when biting?
Neat side note about gloves. I had never noticed going into drawers but tweezers certainly make sense.
Thanks in advance and thanks for running this wiki page! —tkh777
If there is a fracture in the tooth it is likely to get worse with time, avoiding chewing on it should help but often the tooth is put under pressure accidentally by food in that area. It may not be a fracture, it could be a void under the filling or a high spot on the filling or sometimes there is sensitivity of an unknown origin. It is possible that it was caused by the drilling of the tooth but there is no way to know for sure, anytime you deal with a biological system there are many factors that come into play and not all of these are well understood. fractures that are sensitive are often very small and not visible to the eye, if there is a fracture it was not likely caused by the drilling but could have been made more apparent by the work on the tooth. Yes it will often feel similar to the tooth being drilled, a sharp quick electrical type of pain. —DagonJones
2012-11-02 16:00:41 My dentist told me that one of the signs of a cracked tooth is that you feel pain not when you bite down, but when you release the pressure. So, for example, if you press your teeth down slowly on a pencil, it won't hurt, but it will hurt after you let go. Is that right? —CovertProfessor
2012-11-07 15:43:29 yes, that is absolutely correct. —DagonJones
 Decay is outlined in yellow, Filling preparations in Red or Blue 2012-11-08 16:45:01 I am 34 with good health, have had history of sealants only, and tonight I just had a dental appointment for a cleaning. My last appointment 6 months ago the only concern brought up was a Diagnodent (sp?) number of 27 on one tooth (#20) which had changed this visit to a 20. The hygienist mentioned no other complications and then the dentist came up to her at the end and just told her to tell me I needed a couple of procedures he jotted down and she could seal my #20 tooth today if I wanted. So she did the seal and as I am paying she tells me "oh yeah you have to come back for a couple of fillings." She then shows me on the xrays that there are two spots with barely visible shadows between two teeth "across from each other" that will need to be drilled. I was floored because I haven't ever needed fillings before and why hadn't the dentist explained this to me as I had to ask her how do you get to those spots between? She said they will have to drill from above then go to the side...I am just wondering if this is truly necessary or if there is another option? I'm afraid they will cause more damage going after a small spot & could my tooth crack from this procedure? Very afraid...I feel like there wasn't enough info given to me and they act like this is no big deal - like everyone should be fine with getting drilled so what's my problem? She even asked me if I would want gas for the procedure...My problem was the lack of explanation, not the pain of a shot. —LaurieBrown
Decay is outlined in yellow, Filling preparations in Red or Blue 2012-11-08 16:45:01 I am 34 with good health, have had history of sealants only, and tonight I just had a dental appointment for a cleaning. My last appointment 6 months ago the only concern brought up was a Diagnodent (sp?) number of 27 on one tooth (#20) which had changed this visit to a 20. The hygienist mentioned no other complications and then the dentist came up to her at the end and just told her to tell me I needed a couple of procedures he jotted down and she could seal my #20 tooth today if I wanted. So she did the seal and as I am paying she tells me "oh yeah you have to come back for a couple of fillings." She then shows me on the xrays that there are two spots with barely visible shadows between two teeth "across from each other" that will need to be drilled. I was floored because I haven't ever needed fillings before and why hadn't the dentist explained this to me as I had to ask her how do you get to those spots between? She said they will have to drill from above then go to the side...I am just wondering if this is truly necessary or if there is another option? I'm afraid they will cause more damage going after a small spot & could my tooth crack from this procedure? Very afraid...I feel like there wasn't enough info given to me and they act like this is no big deal - like everyone should be fine with getting drilled so what's my problem? She even asked me if I would want gas for the procedure...My problem was the lack of explanation, not the pain of a shot. —LaurieBrown
please read the entry about shallow decay here. If the decay is in the enamel only then some dentists will watch the decay to see if it spreads, so ask your dentist if it is something that can be monitored. Flossing daily will help to remove plaque that can cause the lesion to grow and therefore prevent it from getting worse. The picture below shows an x-ray, decay between the teeth is outlined in Yellow, Red is the outline of the hole that would have to be drilled to access those cavities. The Blue shows another type of cavity preparation that includes the chewing portion of the tooth, this is sometimes done to increase the retention of the filling and/or remove decay on this surface as well. —DagonJones
2012-11-08 22:22:20 Do you have an opinion on those new water flossers? They spray a stream of water between the gums and are supposed to work like floss. Seems too easy... —EricaMacGregor
To quickly answer, if you are referring to the air/water flossers made by sonicare, I am not sure what the research shows but I DONT think they are as good as floss, in fact the manufacturer recommends the product as an adjunct to flossing, not a replacement. I just cant see an air water blast removing as much plaque as mechanical debridement using floss, the floss will cover more surface area as well. If you ask me it is a good gimick and better than not flossing at all but NOT a replacement for floss. —DagonJones
I used my water pic as a nice flush out after I brush/floss. On full blast it's a bit much for the gums, but awesome for blasting stubborn sugar residue / other stuff you don't want posting on your teeth. Never heard of the air ones, that seems iffy Daubert
Water picks seem to be good for removing bacteria that cause gum disease and gingivitis but from what I have heard they do not remove plaque deposits that cause decay, they certainly will remove food deposits that the bacteria use to create cavities. —DagonJones I use floss / brushing and regular dentist visits for plaque removal, or something Daubert
2012-11-17 17:39:29 Is it possible for the roots of your teeth to grow outside of the gums? —dawnheadley  recession
recession
To the best of my knowledge this is not possible, it could be Recession, or a fragment of a retained root from a previous extraction or broken baby tooth that is sticking through the gums.
2012-11-27 22:41:14 Nine days ago I had my second lower molar removed due to pain in previously root treated tooth. I have a wisdom tooth on that side which has never erupted. I am 54. The wisdom tooth can be seen quite clearly on x-ray impacted below the bone. I have been experiencing intermittent stabbing pains in this area on day nine of the extraction. The extraction, although difficult looks like it is healing and no sign of infection. Is it possible for a wisdom tooth to start playing up after all this time and also with no other teeth around it. I am very anxious about this as have rather slot of bad luck when it comes to me and my teeth! I am not in agony just a few stounds going on. —Janiceross
You should definitely talk to the dentist/surgeon who removed the tooth. It is most likely a dry socket or discomfort related to the extraction. It is unlikely to be the wisdom tooth but that is a possibility. —DagonJones
2012-12-29 18:22:30 Dr. Jones, I had adult orthodontics. I opted for crowns instead of veneers for insurance/financial reasons on bottom front teeth, they were very worn down. I currently have crowns w/temp cement, making sure I am content with color before they are glued on perm. Previous color was visibly off and crowns had to be broken off. Both crowns do not cover the entire tooth down to gum line (in the front) and the previous ones did, one is more visible than the other. I am concerned about getting cavities in the area that my teeth are exposed or other major problems as I have noticed in the past couple of days that plaque settles there quickly. I have read that composite would only be a temp fix. The assistant mentioned she had noticed the receding gum on one of the teeth previously. That was the first I had heard of that, I go in for regular cleanings and exams and it is the first I have heard of having a receding gum line (just had a cleaning day before crowns were put on w/temp cement.) I am always told my gums look healthy. I will see my regular dentist next week, she was not the one to temp cement my crowns, the dentist who did it would not give me much information, he stated I needed to discuss any issues with my dentist. I'm nervous, since the prep for molding has been painful both times and it was after the 2nd prep that I noticed how much farther down the temp crown went. On the 2nd prep for molding I could feel the string being pushed into my gum, it was a horrible experience. I just thought my gums had been pushed down and it would go back to normal when I got my crowns. The temp crowns are horrid looking, and since they are on the front teeth and I have a big smile, they are very visible. I dread wearing temp's again. This process has been a nightmare and I had always had good experiences with dentists. I am extremely concerned about gap between gum line & crown, please advice. Thank you. —AliciaGarcia
This a really hard question to answer without actually doing an exam. The area where the crown meets the tooth is called the margin, and it is just fine for this area to be above the gumline, however the margin must be smooth to prevent plaque accumulation. recession can occur even if your gums are healthy, so the fact that no one mentioned the recession before does not mean that it was not there, slight recession (1-3mm) is often not a big deal and sometimes is not mentioned. Talk to your dentist about all your concerns, it sounds like you are having a lot of work done and you deserve to have all your concerns addressed. —DagonJones
2013-01-24 21:47:24 Hey Dr. Jones, have you heard of the Soladey-J3X? I am curious to hear your thoughts on it. —LamsonNguyen I have never heard of this before, but a quick google search explained it for me. I honestly can not say if it works or not but it looks kind of gimicky to me. While it is true that electrons can interact w/ acidic protons produced from bacteria I do not see how that would aid in plaque removal. Bacteria use large charbohydrate-protein complexes called proteoglycans to stick to teath, and I don't see how electrons would interfere with this. —DagonJones
2013-02-17 14:42:26 how often root canals recommended to be changed even if the don't bother and done nicely, i have heard every 5 years
A root canal should not be re-done unless there is evidence of re infection (visible on the x ray) or pain. I have never heard of root canals needing to be re done just on a routine basis.—DagonJones
2013-02-26 09:25:39 Hey i am 20 year old college student who has never had a cavity and brushes and flosses everyday. Last week one of my teeth had started to become infected/absess. This infection has now spread to the front of the beginning infected tooth and the rest of my lower front teeth. Along with one of my top front teeth. I have a small sore on my tounge and have a streptococcus infection in my throat now. Please help me my teeth are going down the drain fast. —henryberns
It sounds like a gingival problem based on your description. you should see a dentist soon, if you are an undergraduate at UCD you probably have dental insurance and an office visit will likely be covered at about 80 to 100%. be sure to continue to brush, floss and use a mouthrinse like listerine. Gingival infections often get worse if you do not keep the areas clean, but it is a good idea to be gentle. you could also have herpetic gingivostomatitis which I believe is more common in your age group. feel free to call my office 530-756-5300 and ask to speak to me directly if you have specific questions about this. —DagonJones
2013-04-01 12:07:30 Do I really have 4 choices? Consultation revealed 3 options: (1) Nothing, (2) Implant, (3) Post and Crown lengthening. My internet searches unvieled a possible fourth: (4) Forced Eruption. Background: My root-canaled #19 will no longer maintain it's crown. Care to discuss? —StephenASiracusa
I need a little more information here, is the tooth root canal treated? In most of these situations part of the tooth broke off inside the crown and there is not enough tooth structure to maintain the crown. The best and most predictable option in these cases is extraction and an implant. Crown lengthening is a decent option but it involves removal of bone that you might need later if there is a failure with this restoration. forced eruption is difficult on a lower molar (#19) and would not likely get good results due to the large surface area of the roots on this tooth (consult with an orthodontist). I hope that helps.
2013-04-09 12:18:36 Thank you for the reply, and yes, #19 was indeed root-canaled. Also thank you for the insight, re; future options. I didn't consider the negative result of bone loss and how it may impact future implant success (or failure) if I eventually need an implant. But at least I now know that forced eruption is not an option. —StephenASiracusa
2013-04-23 05:04:49 Alright - I have been thinking about making my own toothpaste. Some things I've read say that baking soda will hurt the enamel of the tooth, while others don't mention it (and of course, no one cites any science on the internets, it seems). What do you think? —ChristyMarsden
I think you should just buy toothpaste, there are so many options to choose from. Store formulated toothpastes have all the good stuff in them, fluoride to protect from cavities, detergents to help clean off plaque, and abrasive particles to remove stains. Baking soda is a very good cleansing agent but it is a bit too abrasive for every day use, if you use it every day it can wear down the enamel a little too quickly. Many toothpastes have varying degrees of abrasiveness, it all has to do with the particle size of the abrasive agents. Most toothpastes that claim to be "whitening" do so by having more abrasive particles to remove stains better so they are often not indicated for daily use. If you want fluoride free toothpaste (which I personally don't recommend) or all natural toothpaste then use Tom's brand, it is pretty good. —DagonJones
Thank you so much, DagonJones! I miss having you as my dentist ... I'm ashamed to say that I haven't been to one since I left Davis because I'm not sure any will be as good. But I'll get the normal toothpaste (whitening makes my teeth too sensitive) and keep flossing away. I very much appreciate your knowledge! —ChristyMarsden
2013-05-22 16:05:21 Dr. Jones, thank you for your help! I've had tooth pain around #2 for months. It was on-off, sharp pain w/ sensitivity to cold and hard food. Relieved with NSAIDs. I went to a new dental practice in Jan (4 months ago) for a focused exam with the chief complaint of "cavity." At the exam, no films were taken and the dentist found nothing unusual on exam except for minimal recession that he said was likely not contributing. In fact, he explicitly said I do not have a cavity. A few days later, I went for a new patient comprehensive exam & cleaning. Again the complaint was brought up, a different dentist at the same practice took a look, and also blamed the slight recession for the pain. A full, routine x-ray panel was taken that was unremarkable.
Two weeks ago, the pain became more severe such that sucking & smiling widely hurts and the tooth is more sensitive. Two days ago, I noticed foul odor from #2. I went to the same dentist this AM and he took an xray of #2 that revealed significant decay of the distal surface confirmed on exam. The dentist (mid-30s) said he had never seen decay in that spot before (on any patient). The excuse was the decay was partially hidden by gum and not captured on the comp exam x-ray. The root cause was theorized to be due to maxillary bone loss s/p wisdom tooth extraction that left #2 vulnerable to decay. The dentist charged me for the encounter (insurance had paid for the prior two not helpful exams) and referred me for root canal.
Will dentists typically charge for an missed diagnosis leading to an additional non-insured visit? And is this type of missed diagnosis routine or should the dentist have taken more responsibility? Is the insurance company the party I should complain to in hopes of getting reimbursed? —EricKing
The type of decay that you are describing is notoriously difficult to diagnose, there is a natural concavity on the back of most 2nd maxillary molars and decay can get rather deep in this area and look within normal limits on an x ray (there is naturally a dark spot on the x ray here), and due to how the gum tissue often sits the decay can be under the gumline and not visible on routine visual inspection. So I don't think it is due to any lack of skill by the dentist, regarding the difficulty in discovering this decay.
The question about billing and insurance is a difficult one to answer, what you insurance covers is totally up to the insurance company. These are private for profit companies, it is often in their best financial interest to not cover anything outside of what is "ordinary" for 80 % of the population (I am just guessing at that number). What your dental practice decides to charge for is up to them as well, there is no standard of care when it comes to billing practices. Because fees account for the practioner's time, expertise, and clinical guidance, a practice will often bill out for these services every time a patient is scheduled for an evaluation. Some practices will not charge for a second follow up appointment when it is related to a recent previous evaluation. These decisions are made by the practice based on their desire to establish and maintain goodwill and receive compensation for the services they provide. I can see both sides of the situation here, I understand your frustration for having to pay for the diagnosis of a problem that was not discovered on the previous exams. However every exam will not discover 100% of pathology 100% of the time. So I understand the justification for billing for services when the practitioner was using sound clinical judgement, even though this area of decay was not discovered in a previous evaluation.
I recommend you call the dental office and talk to them first about your concerns. —DagonJones
2013-06-13 02:35:20 Hi, i am 43 years old, recently i contacted dentist as i dont hav wishdom tooth and other one tooth. i need to put new teeth agaist this. i have also gaps between three gaps (in downline) as it is not much but i dont like. she suggested bridge/crown treatment. she called me and as i dont know the procedure, she started reducing my teeth, after one tooth i realized that my natural tooth are reducing for this treatment, she had done this with my all front teeth. now she called me after one week for trail of cap / crown. if i dont want what can i do as she already reduced my teeth..what will be the procedure for crown treatment, is it good or not as i dint have any pain nothing. is there any problem after crown treatment in eating or anything...pl reply me —anju
you are committed to some type of crowns now that your teeth are reduced, however if you are not happy with the appearance of the crowns before they are cemented just let your dentist know and she will be able to change the shape and color with the lab. There should not be any problem after crown treatment, if you are not having any sensitivity now you are not likely to experience sensitivity. Crowns cover the reduced teeth and replace the removed tooth structure, they can break or get decay under them but if they are well cared for they should last decades. —DagonJones
2013-06-14 08:00:09 I had my wisdom teeth extracted about 6 years ago. The oral surgeon punctured my gums and caused a severe infection which almost killed me. It included the infection bursting in my mouth, lockjaw, not being able to eat or drink. I went to him several times and he told me it was tonsilitis as he's prying my mouth open. Anyway, I had to see a ear, nose, throat doctor and as soon as he looked in my mouth rushed me in to do emergency surgery. I had an infection in my whole mouth which was beginning to spread down my throat and headed to my brain. Ever since this time, whenever I get any type of toothache or abscess it feels like my whole jaw hurts. It also affects me physically. I am physically fatigued and just feel sick all over. I normally have to get stronger antibiotics than just penicillin. When I have had other teeth extracted in the past, it takes me a longer period of time to get over the extraction and usually have to have another round of antibiotics. What is wrong with me? Am I just crazy? My dentist doesn't seem to understand when I try to explain this to him. —RaneyMiller I cant say but you may have some latent infection in your jaw, this is a difficult thing to evaluate and I would recommend seeing an oral surgeon and getting a 3D icat scan (a 3D x ray). The fact that you feel fatigued would suggest a latent infection, the pain in your jaw from toothaches could be residual nerve damage. I am not sure, your whole situation is not something I am familiar with. I would consult with an oral surgeon or a TMJ specialist. —DagonJones
2013-06-19 03:22:27 I have a 14 years (running) old son and 7 years old daughter. i thought my son has teeth little bit outside, i consulted dentist but they advised me that you wait for 2-3 years as he is small, he will be ok as he time goes, pl tell me if i want to put him braces when should i do..... for my daughter she has her two last teeth downline totally damaged ( i dont know exact word, as she eats more chocolates and all, both last downline teeth are black and i think it shd be removed. pl advise me what is the treatment they require... —anju
2013-06-22 00:11:37 this is further to my question on 13 june. my doctor placed temporary crown and also both side missing tooth with bridges. first of all all teeths are thick, i dont feel comfortable, i cant chew food. it dont match with my upper jaw... i fear now how can i eat as i dont have any natural teeth in downline as remaining teeth were reduced for crown and bridges...also temporary crown come out after 3 hours. pl i need yr advise, and tell me after crown, bridge treatment i cant eat as earlier...i am scared i feel very depressed.. —anju
I am very sorry but I cant answer your questions over a format like this, I would need to do an evaluation on you and your children to understand what the specific issues are. I can say that bridges often take some time to get used to, they feel very different at first but after a few weeks you should adjust to them. It is also possible they do not fit well and need some adjustment. Call your dentist for a consultation they will often not charge for an appointment like this. you have many questions and you should take the time to discuss your concerns with your dentist. —DagonJones
2013-06-29 02:49:45 I just had fillings done on 3 of my teeth on my right top side. I was not having any pain when i went to have this done. It has now been 3days,and one of the thooth i had worked on is hurting me real bad. It is waking me from my sleep. I am taking tynol for pain. I was wandering if this is possably normal, or do i need to conntact my dentist? My teeth are also now very sensitive. Hot or cold never bothered before, but now i am having problems chewing my meals that are hot, and things that are crunchy. I have had fillings in the past. I did not have any of these problems. Thank you for any advise! —RebeccaHardin
Sorry everyone, I was on vacation last two weeks. Pain after fillings is unfortunately rather common and considered normal. sensitivity to hot and cold is especially common. However if the pain is waking you up at night it is possible that the decay was very close to the nerve in the tooth and it is possible the tooth needs a root canal. If the decay was very close to the nerve then the nerve can be irritated by cleaning out the decay, of course if you did nothing the decay would eventually reach the nerve and you would develop an infection. My advice is to wait 2-3 weeks, the pain should start to diminish if it does not, call your dentist for an evaluation for a root canal. —DagonJones
2013-07-01 16:06:02 Dr. Jones - On Feb 9, 2012 I had both upper wisdom teeth and the molar in front of the upper right wisdom tooth extracted by an oral surgeon. My dentist had determined that the three teeth had to go because of decay below the gum line. Within a few weeks of this procedure I began experiencing dry mouth and to a lesser extent burning mouth with no interruption or improvement in the symptoms to date. I have been seen by my family doctor, two ENT's, a different oral surgeon, and my regular dentist with really nothing to show for these visits and no improvement. I have been tested for Sjogren's, thyroid function, kidney function, and whatever else blood can be tested for. I do not take any Rx medicine. I guess my main question is what exactly might be causing my symptoms and do the symptoms probably relate to the tooth extractions. I recently became aware of a condition called Occlusal and/or Oral Dysesthesia which seems like a possible cause. I also haven't been checked for a possible neurological cause. I'd like to know what you think might be the cause and also what your advice might be re what treatment to pursue at this point. Thanks —TomKoester
I wish I had an answer for you, however I do not know what is causing your symptoms. I would assume it is something that is not clearly understood. Human biology is incredibly complicated especially when it comes to sensory issues. It sounds like your health care providers have done very good due diligence when it comes to checking for all the known issues that could be causing your symptoms, the fact that nothing was discovered is frustrating. It is possible that it is related to the extractions but I could not say for sure. Regarding oral Dysesthesia this seems to be a catch all term for idiopathic (from an unknown sorce) oral discomfort, there is also "burning mouth syndrome" which may be an adequate way to describe your condition. The best you can probably do is use different products to alleviate the discomfort, there are a variety of dry mouth rinses/ sprays that you might try. The burning sensation could be secondary to dryness —DagonJones
Dr. Jones - Thanks for your prompt response. "Idiopathic" does indeed seem to be the key word to describe this stubborn problem I have. I am thinking of trying to get in to see an oral pain specialist at a state university dental school a few hours from where I live. Do you see this as a logical and worthwhile course of action? Again, thanks for your prompt and thoughtful response.
2013-07-02 09:39:05 I'm 72 years old and have all my teeth, with exception of four molars extracted when in my early teens...either side, top and bottom. My last filling was some eleven years ago. I always clean my teeth morning and night. I do not suffer any regular or periodic toothache. However, since moving to Spain seven years ago my regular diet is to eat a mix of fresh fruit each evening....banana, orange and apple mix. I now notice that my gums are receding and one back tooth is quite loose. Should I adopt a different late night supper mix???? —BarryWootton
It is incredibly unlikely that the fruit is causing recession and loose teeth. most likely this is due to periodontal disease, which often gets worse as time goes by. Genetic predispositions for periodontal disease are much more active in the later half of life. I would highly recommend you see a dentist for an evaluation and commit to periodontal treatment and very regular periodontal maintenance (cleanings). Even if you care for your teeth very well at home a professional cleaning is essential to maintaining health because the hygienist uses instruments to remove deposits that cannot be removed at home. You may not have periodontal disease, some recession comes from a variety of other causes ( age, vigorous tooth brushing, heavy clenching, naturally inadequate thickness of gum tissue ) but the loose tooth is often an indicator of periodontal disease. —DagonJones
2013-07-12 04:03:02 Dr. Jones, I recently received a gold implant to replace a fractured back lower molar. It's a snug fit and I'm very happy with it. However, the gold has a small sharpish point that sticks out laterally into my tongue a little, which the dentist left on purpose - he said my tongue would get used to it. Indeed it's starting to annoy me, but it's only been a day. Can you explain what the purpose of leaving this little point might be? —BobEggerton
I dont know for sure, it is probably due to the contour that is necessary to meet with the opposing tooth. An implant has a smaller base than a natural tooth, therefore the shape of the tooth has to have a more pronounced taper and this shape change is probably what you are noticing. It might be possible to smooth it off if it continues to bother you but wait at least 1 week to allow you time to adapt. —DagonJones
2013-07-15 17:39:09 Hello Dr, I noticed a light tan/brown round spot on one of my big front teeth, very oval shaped and nearer to the top portion of the tooth. It somewhat came on quickly.. maybe over the course of 2 or so weeks. I know I should not have but I scraped it a bit because I thought it was a stain. The coloring is gone, but there is an indentation of where the stain was, also (which i expected) my tooth feels sensitive now. Is this really really bad? I haven't been to the dentist in a long time. I have tried to google what this might be but haven't found any answers yet. I don't know if the enamel is completely gone in this area to what but you can tell it is a different type of texture then the rest of my tooth. I am kinda freaking out that I ruined my tooth. Any help would be great. —sarahstewart
If you can post a picture or email it to dagonjones at gmail that would be helpful. there are a couple of situations this could be, either it is calculus (tarter ) that formed there and you scraped it off, or there is some decay on this tooth, or you have some recession that exposed some of the root surface of the tooth. The root surface is naturally darker and more prone to staining, and it is often very sensitive to touch so this is probably what is going on. if you scrape the root surface hard enough you will remove some of it and increase sensitivity but this is not the end of the world. Try using some sensitivity protection toothpaste for a few weeks and that might help. It is probably best if you see a dentist because you might have a cavity here that needs a filling. Don't worry too much you probably did not cause any irreversible damage. —DagonJones
2013-08-13 12:10:40 I am currently part way through a course of dental work including five implants and replacing a number of crowns. A number of these crowned teeth are already root filled and though my dentist says this root filling work has been of good quality he wants to re-do the root fillings before he replaces the crowns. He says he can't guarantee the new crowns unless he does this. Could you give me your view on the advisibility of disturbing root fillings that have remained in place successfully for a number of years? Would it be better to leave them alone? I would value your opinion. A. D. —AmandaDavidson
2013-08-18 18:14:40 I personally would not plan on re doing the root canals unless there was evidence they were failing. It is unlikely to cause any problems by re doing the root canal. It sounds like your dentist is advising a "better safe than sorry" plan for these teeth and if you are going through a very detailed and comprehensive treatment plan this may be a good idea. However re treating a root canal before a crown is not normally necessary. If the root canal fails after the new crown is placed then a hole can be drilled through the crown to do the root canal, this hole does not often significantly weaken the crown unless it is an all porcelain crown. —DagonJones
2013-08-18 09:57:35 i have a crown on my lower incisor with another crown second molar back and a bridge between. About three weeks ago I started having tooth pain in that area, that continued to worsen to the point of going to the ER. Was prescribed something for the pain and amoxicillan 875 bid. Three days ago while eating pound cake of all things, my crowns/bridge fell out. I no longer have dental insurance, live in a different state than before, am in severe pain and my jaw is swelling. Dont know what to do. feels like a nerve is exposed. The ground down teeth are both black in color. Is that the way they were prepared before crowning? HELP —tammyginn
The black color is likely due to decay (but can also be just non problematic staining), the swelling is likely due to infection. You probably need to have one or more teeth extracted. I would recommend you see a dentist as soon as possible, if infection is involved then this situation can be very serious. Do a google search for local community dental clinics or dental schools if your finances are very tight, you might be able to save some money this way but it will likely take more time. If you can't get to a dentist soon then you should go on another round of antibiotics ( go to urgent care) but keep in mind that antibiotics will only keep the infection down for about 3 weeks. —DagonJones —DagonJones
2013-08-18 22:26:10 I recently had my 6 mo. checkup. When completed my dentist said that he could do a little bonding to three teeth if I wanted him to do so. The procedure was very minimal and was totally (all three teeth) completed in 10 -15 min. The bill came in the amount of $435.00. Can this be right??? —JanisWingate
Yes that can be right, minimal bonding is often a very quick procedure. A proficient dentist with well trained assistant can achieve very nice results in very little time. Sometimes a procedure can have a relatively low fee and take a very long time if access is difficult and the decay is extensive. Dentistry is commonly billed out by procedure, not an hourly rate. Fees are determined by the type of filling material, the number of teeth and surfaces involved, three separate one surface fillings will be more than a single tooth with three (or more) surfaces. Composite fillings have higher fees than amalgam because it is more technique sensitive and has more steps involved.
2013-08-26 05:35:31 This tooth is a molar and was root canal . it was not effective and eventually the crown broke and i had to extract the tooth . Now after 2.5 years there is a small hole in my gums in the place of the extracted tooth and is sensitive. —deborahperez.
It is possible there is an infection in this area and the hole in the gums is a small area where pus is draining out of. See a dentist and get an x ray to be know for sure. -Dagon Jones
2015-08-20 16:57:15 i have a piece of tooth traveling in my gum and it causes massive pain but my dentist is on vaca rightnow and other dentists don't like finishing jobs that were not done good by other dentists...what to do??? —Mar
Mosts dentists will by happy to address this issue for you, it often requires simply numbing the area and removing the small piece of tooth, you may need to see an oral surgeon. - Dagon (sorry for all the late replys, I am not very active on the wiki anymore)
2015-10-11 19:36:25 Can braces kill the root of a tooth in adults? —goldie253
It is very unlikely for orthdontics to cause the nerve to die within a tooth (but it is possible, I have never seen it first hand). Braces are more likely to cause root resorption (blunting of the root tips). This resorption usually is of little consequence, however if it is very severe it can reduce the amount of root that supports the tooth and create a situation where the tooth is more likely to become loose if there is trauma or gum disease (periodontitis). Good orthodontists keep a close watch out for situations like this and will let patients know the likely risks. For the most part modern orthodontics are very very safe. -Dagon Jones
2015-10-16 08:07:40 hello...would you please answer my question...i am really worried about my teeth.... my first incisor tooth of mandible showed this unique problem....i don't know how... its crown has popped out and its root has popped inside exceeding the lower bone line...actually now i am wearing braces...would you please tell me what problem is this...my dentist said we should extract that tooth and replace it by fake tooth....i really don't want to have fake tooth at this age...i am very young for that...please help me.... —Kusumpoudel
I am not sure what you are saying here but it sounds like it might be due to the braces, sometimes if the bone around the front teeth is very narrow the tooth can actually orthodontically move into a precarious position in the bone and require extraction. -Dagon Jones
2015-11-15 14:44:58 Dentist thinks tooth is infected and wants to pull it. I have no pain at all so if it is really infected wouldn't it be sensitive and painful? —Libby
Many times a tooth can have a significant infection and you may not feel anything at all. If the infection can drain then it may never be painful. The tooth may not need to be pulled, it might be able to be saved with a Root Canal Treatment.-Dagon Jones
2015-11-17 10:10:13 I am 73 years old I am having my top teeth removed do you recommend bone replacement graft for rid? I am getting dentures thank you —wandasq
I would not recommend bone replacement as a standard for dentures, often there is enough bone for dentures. However some cases require bone grafting but this is not the norm.- Dagon Jones
2015-12-06 23:49:52 I have a new, very uncomfortable upper partial that my dentist thinks might be better if I have much of the metal cut out leaving a metal band across the front and a small band across the back. Is this a good idea? Would it allow me to eat comfortably and not get food under the partial? Thank you. —clarissap
I am sorry I can not answer this question without examining the partial and your mouth. -Dagon Jones
2015-12-11 07:11:32 My daughter damaged her tooth during basketball. They started the root canal process and put whitener in because of blackening of the tooth. Suppose to go back next week to finish procedure but patch on back of tooth fell of. Dentist offices in our town are closed on Friday and all weekend. Can she eat and drink. She is worried about whitener. —fish1
She should rinse out mouth well with water to remove the whitener (bleach), then brush the back side of that tooth to remove any remaining bleach, it is better if that is not swallowed. She can eat and drink but should brush the back of that tooth after eating or drinking to remove food that might get caught in there. Get a new temporary filling as soon as possible. -Dagon Jones
2015-12-21 14:40:26 Hello, I was wondering, if there is two cavities on one tooth, is it normal for dentist to charge for the same tooth twice with different number of surfaces? Shouldn't it be just one charge per tooth with all surfaces counted together? And other question: Is it alright to do surgical extraction of erupted molar(partially broken, but simple roots) and then charge for that and alveoloplasty?(didn't ask me about it or future dentures plans) Thanks! —lucy85
Every dental office has different billing procedures and policies so it is hard to say what is "normal". As a rule I prefer not to answer billing and insurance questions. Sorry those are more legal / business questions and I prefer to answer questions about dentistry itself. -Dagon Jones
2016-01-19 15:39:45 my daughter had silver caps for 3 years and one is loose and bleeding —shanel
The tooth is probably a baby tooth and ready to come out naturally, I would not worry too much about this but I would have a dentist take a look at it.
2016-01-21 22:47:05 Hi, Dr. Jones and any other dental professional, Thank you for all the advice you have already given on this page! Some gum tissue around my lower left-side teeth have been sore for the past few days. I have been told that I have tooth recession in the area, and the gum tissue around the sorest area has receded pretty far down below one tooth. I went to the dentist last month and she replaced a filling in the tooth on my request. It seems likely, at least to me, that the pain is due to gum problems, not tooth decay. I am finally going to call the dentist tomorrow and schedule another appointment, but had a few questions in the meantime. I am mainly wondering what else I can do to prevent gum recession. I really try hard to take care of my teeth--I brush twice a day with an electric toothbrush for at least 2 minutes, I floss daily, I use fluoride mouth wash. This is why I am surprised that I am having gum problems. Anyway, I am wondering what else I can do to stop the recession, namely... My electric toothbrush--perhaps I am brushing too hard? I try to hold it gently, and let the electricity do the work. I'm not really sure if the bristles are hard or soft, because I just buy the Oral B replacement heads. Any thoughts? Dietary habits. I'm a grad student and drink lots of coffee every day, perhaps too much. Could this have an impact on recession? Again, thank you for all the help; I really appreciate it. Eric Jensen —EricJensen
Some people get recession more than others and there are probably genetic factors that come in to play that I am not aware of. The most significant environmental factors that make recession worse is vigorous tooth brushing with a firm or medium tooth brush (oral B electric heads are soft). Avoid long back and forth strokes when brushing along the gumline, it is better to use gentle circles or very short gentle back and forth motion. The key to good brushing is to be diligent but not force full. Electric tooth brushes do a lot of the work for you so you just need to hold it against the tooth with gentle pressure. Clenching your teeth is also related to recession so avoid clenching if you can and wear a custom made night guard to prevent night time clenching. -Dagon Jones
2016-01-27 21:28:59 I have temporary crowns can I change my mind and have them removed? I have had them for six days now and can't stand the way my mouth feels, constant headaches ect. Thank you in advance for any help you can give me. —jimd
Talk to your dentist about your temporary crowns and your pain, I can't advise you on this issue without a detailed exam of your situation. -Dagon Jones
2016-02-21 09:51:04 So here's a question- I went in and got a root canal done about 2 months ago. A couple days after the procedure it was apparent that the left side of my tongue was still numb and I couldn't taste. The dentist said it was a long healing process. After hearing this I jumped online and researched and found out that what I have is LNI.. I don't know if it's permant or trying to heal.. But ever since the procedure I haven't been able to floss behind the repaired tooth-it's too tight there is no space for floss.. It also feels tight to the next tooth.. So I was wondering if the pressure might be causing the numbing and/or lack of healing —Sbpw88
Nerve Injury during dentistry is very uncommon but it is possible this occurred during the numbing process for the root canal. Situations like this almost always heal back to normal but it may take several months (sometimes 6+ months). The difficulty with flossing is probably due to the temporary filling that was put in after the root canal. You should have this replaced with a crown as soon as possible otherwise the tooth is likely to break. Once you have a well made crown on there you should be able to floss just fine.- Dagon Jones
2016-02-29 07:39:38 Hi.i have very bad gaps in gums i dont like going out..if i got my teeth cleaned would it make the gaps worse and could i get something done about the gaps. —sarah07
The gaps in your gums are likely from periodontitis (gum disease). The most important thing to do for periodontitis is to get regular cleanings, you don't want to let the disease get worse because it can cause tooth loss and is connected to overall body health. People with untreated gum disease have a higher risk for diabetes and cardiovascular diseases. It is possible that the gaps get worse if you get a cleaning, this is because after a thorough cleaning the gum tissue will be healthier and less swollen which can increase the size of the spaces not filled up by gum tissue. There is cosmetic treatment that can be done to fill in these gaps, unfortunately it is often extensive dental work involving crowns. Sometimes these gaps can be filled with less extensive dental procedures such as white (composite) fillings. -Dagon Jones
2016-03-06 08:00:21 Hello I am wondering if you could help me. I have had quite a bit of dentist work done recently and it's been one problem over after the next over the last year. I have recently developed sensitivity to cold on my front tooth. I have a composite filling behind this tooth. At my last appointment I mentioned it to my dentist and he said sensitivity is quite normal to cold etc and he checked that the filling was still intact. Since this appointment a few weeks ago the sensitivity has increased and it almost feels bruised on the side the composite filling. It's not sore to eat, I don't have a pain that wakes me up at night but it is tender to touch with my bottom tooth . I don't have an appointment until next week and I am so very worried that I am going to need a root canal on this tooth. Also, I have had for quite a few years a translucent patch on the front of my tooth that is visible when I look very close in the patch at the tooth where the white filling/composite is but I have always assumed it was just weak enamel but it extends from the edge inwards. I am now concerned that this is infact decay but I find it difficult to understand that this would not have been picked up. Any advice would be much appreciated and if you think that this could be an infected pulp - is there any chance this could be rescued if I see someone? Would there be any other explanation for my symptoms? Thank you —josiet
It is hard to say without a thorough examination of your tooth, but it is possible that the tooth is in the early stages of nerve deterioration that could result in the need for a root canal. However, based on your symptoms it seems more likely that you are simply experiencing some transient normal sensitivity. The translucent area you are describing is probably the composite filling material itself, that material is often more translucent than the tooth. If it was decay it would have a brown appearance with bright opaque white at the edges (sometimes just this bright white with no brown). -Dagon Jones
2016-04-05 10:45:08 I recently went to dentist and he I have a root tip on a previously extracted eye tooth that he wants to extract now. I have never had any problem with this and it was done 10 yrs ago. Should I have this done? —kathyr
I can not really saw without seeing an x ray. But as a "rule of thumb" if the root tip is surrounded completely by bone and there is no radiolucent (darkness on x ray) area around the root then you should probably just leave it. A radiolucent area would mean infection or cyst and then it should be removed. -Dagon Jones
2016-04-10 01:30:34 Yes during my dental work I woke up to see thie Dr. Was putting a small needle like about an half in. Had red on one end and blue on the other into my tooth I know it's in there I have felt it and I want to know what was it and why do I have it used for —Sylvia1966
- That could be a post, a root canal file, or an injection syringe for anesthetic (all normal and nothing to worry about). Sorry, but I can't say more without seeing the actual item or knowing what the procedure was. - Dagon Jones
2016-04-20 09:08:56 I had major dental surgery over a month ago. I have had complications and infections for over a month. The dentist has repeatingly have me taking antibiotics for over a month. # 8 tooth was extracted, with a bone graph, the graph dropped and the sutures came loose. One of the dentist just told me a nerve has been interrupted on the #7 which caused nerve damage. I was told yesterday I have to pay out my pocket. The dentist was paid over $7,000 to complete the work for the implant and bone graph the procedure is not finished at this time and I have a missing front tooth. I am in such fear of this dentist that I can't go back because of his poor work ethics. What do I need to do? —sporter13
I am sorry, but I only answer questions about the specifics of dentistry itself. This is more of a legal/ ethical question. Issues like this have many variables and would require a lot of detailed information from several parties to evaluate, unfortunately this kind of thing is just not my forte. I wish you the best of luck and you may want to consider contacting an attorney. You also may simply call the office and voice your concerns, many offices will work with you to make you comfortable. - Dagon Jones
2016-05-28 19:45:25 Hi, can you please tell me why I was born with multiple missing baby teeth (4 bottom teeth all side by side as well as another one or two elsewhere in my lower gums) there were just none of these teeth in the gums. As well as this there were other teeth in different parts of my gums but there were only primary teeth, no permanent teeth were present. Unfortunately this was always considered a minor issue as for most of my life including now i I have been extremely ill. My bottom teeth are the big issue as there is very little bone. My top teeth are not as bad I was able to get some bridges and crowns. However I believe I would need bone grafts in my lower gum to allow for implants aswell my jaw broken in order to give me a proper bite. Can you tell me would this be risky for a person like me who has had multiple life threatening surgeries and another due in a few weeks. If this isn't an opion that you would recommend can you please tell me what other options are available if any that would allow me speak and eat in public, without always feeling terrified someone will notice them. This has been an issue all my life and if I survive my next op I would like to finally try to fix my teeth properly. I would really like your opinion and I would like to thank you in advance for giving me the opportunity to seek advice from you. Kind Regards, Emma —Emmamargaret
Congenitally absent adult teeth is a relatively common situation. You do have options to replace these teeth but your options depend upon your individual situation and would require a full exam from a dentist. Your overall health would have to be considered as well. Sometimes implants can be done without the surgery to correct your bite, the surgery to place implants is very simple but surgery to adjust your bite is more involved. If implants are not an option you probably could have a removable appliance made that would fill in the spaces with false teeth, These often look very nice and are comfortable after an initial phase of getting used to them. - Dagon Jones
2016-06-07 16:47:55 I am middle aged and have *never* had a cavity or dental issue (aside from childhood orthodontia). I understand the need to do radiographs periodically, but I object to doing them on general principle every year or two. Is there any reputable dentist in the area who will have me as a patient without insisting on (bi)annual x-rays? —damsel
There is no written standard for how frequent x rays should be taken. It all depends upon your individual risk for decay and the health of your gum tissue and bone. Screening x rays (aka Bite wing x rays) not only check for decay but they are also used to monitor bone levels. I have some individuals in my practice that are on a two year interval for screening x rays, and one or two people who are on a 3 year interval. However the vast majority of people benefit greatly from an annual interval. If you call and ask to speak the the dentist they will often be willing to have a discussion with you about their opinion on x- ray interval frequency. -Dagon Jones
2016-07-04 20:13:00 I have an infection in my lower left jaw from 3 bad teeth. My question is what type of sedation is generally used for having 3 teeth extracted, deep Cleaning, and 3 posts in one visit. I have to say I had not been to the dentist in 30 years as I am terrified to go. I went because the pain was so severe I was actually getting sick. I have been on an Antibiotic (Clindamyocin) and Hydrocodone for 4 days now, and still feel horrible. I asked if I would need to have a ride to & from the appointment, and they said No, as they will only numb the area they work on so I will be able to drive. Now I am even more worried and sick to my stomach that it will all be to painful to have with just Novocaine. What is your opinion? —Itsdaky
Every dental office will offer different levels of sedation. Most of the time simply local anesthetic is all that is needed. However for individuals such as yourself who are extremely nervous or phobic, oral sedation with certain relaxing medications can be very helpful. Some offices offer IV sedation and you can have very deep levels of sedation where you will not remember anything, this type of sedation is much more common in Oral Surgery offices and less common in general dentist offices. Call the office you are working with to discuss what levels of sedation they offer. In my practice I often use Triazolam sedation for nervous patients. Triazolam is an anti anxiety medication (in the same family as Valium) that helps relax individuals. This medication does require that the patient have someone else drive them to and from the dental office because it does impair you ability to drive. - Dagon Jones
2016-08-18 03:59:38 Tooth Extraction For Immediate Denture: Is it normal procedure to saw the teeth off at the gum line and use a scalpel to cut out the rest of the teeth below the gum? 20160711_063204.jpg —msteri
Your perception of what occurred is likely different from what actually happened. Certain teeth may need to have the crown (the part of the tooth above the gumline) removed or sectioned into pieces before the roots are extracted. The crown is often removed with a dental handpiece ("drilled off") then the remaining roots are extracted using instruments called elevators. These elevators are are small instruments that loosen the root from the bone and help elevate them out. In order to gain better access to the roots, incisions may be placed into the gum tissue using a scalpel. However, a scalpel itself would not regularly be used to remove the tooth. Afterwards some sutures ("stitches") may be placed to close up the gums. -Dagon Jones
2016-09-01 01:27:41 I have a 2 year old daughter. She has a growth hormone deficiency and her teeth have been slower to erupt. Currently her canines on the bottom appear to want to come through the front of her gums and seem to be down lower than I remember a normally erupting tooth to be. Is this something to be concerned about or should I just give it time? I'm very grateful for your willingness to answer questions. TIA. —HDrans
I would not worry about a situation like this, even if the teeth were erupting from an unusual location, they will often migrate into approximately the proper position with time.- Dagon Jones
2016-09-09 06:25:58 Throughout the years, I lost all the teeth except #22 plus another one on the other side next to a lost molar on my upper jaw, following advice of dentist with one unethical one on alleged decay diagnosed by X ray. Following the unethical dentist, I found a very honest one for about 6 years. He let me keep the teeth even though one showed very weak via X ray and started to get loose. That tooth lasted 15 months after he suggested extraction, because I have finally to clean very well with perio-aide attached to a good flat tooth pic to scrap buildup + Waterpic flosser, regullar florsser + Plax + Hydrogen Peroxide rinse no less than twice daily with concentration equal to Colgate Peroxyl. 15 months ago, I had 2 implants initiated with one regular size implant about 4 mm or so next to Tooth #22 plus another one the other side of the month. The one near by #22 some human bone powder was added. 10 months ago, after first exposing the implant, a custom made partial to be hooked to the 2 natural teeth + 2 implants was implemented. 3.5 months later, a new regular dentist claimed that there was decay according to X-Ray and advised extraction. A second opinion concurred. The prothodontist who engineered the implant + the custom made partial also suggested extraction because he sold the practice to a Romanian prothodontist upon his retirement. The tooth is NOT lose, everyone agreed. There is no pain and no pus but some redness on tissue nearby,. The implant - partial has been working well. I got one missing screw on the partial replaced by the dental lab of another dentist (my current one). He advised extraction whenever there is any sign of decay via X ray. I told him not to worry about his alleged "blood poisoning" from decay because I have some medical background as a retired clinical chemist specializing in endocrinology and clinical toxicology PLUS 2 M.D>'s agreed that the Sinus is blocked for adults and therefore there is zero risk for toxins entering the passage to the brain. I really hate to have the #22 extracted because all agree that the chewing power is expected to be decreased with loss of the tooth and past histories show the alleged decay tooth can last at least 15 months. I am 74 years male. What is the probability of the bacteria from the alleged decay of #22 start to poison and then kill the implant about 4 mm away spatially ? Should I get a 3rd or 4th opinion from the honest but clumsy dentist who taught me how to clean teeth well with perio-aide attached US made flat tooth pic so that all the debris and buildup can be literally gently scraped away? Are nearly all dentists believe that extraction is needed whenever the X Ray shows decay? THANK YOU SO MUCH DR. JONES. —johnking
Tough to answer for sure without looking at the x ray and the tooth. Even if the tooth is not loose, it could have extensive decay that makes it difficult to restore. If the decay is deep enough it could lead to a dental infection if left untreated, It is rare for these infections to be life threatening but they can be a significant drain on your immune system. If it develops an infection it could compromise the implant next to it. I would simply ask the dentist that you trust if there is any way to save the tooth, if the answer is yes, then ask your dentist if they think it is a valuable tooth to save. Perhaps your denture will fit fine without this tooth. In some situations a tooth like this can be root canal treated, then a "zest locator" attachment can be placed in the root to act as an attachment for the partial denture. (see the photo) -Dagon Jones
Add a caption
2016-09-24 22:41:48 Hello, I am quite confused. I visited a dentist a year back, he told me, my teeth's are absolutely fine. Last week, when I had small pain in my jaws, I visited another dentist, she told I had six cavities out of which four can be filled up and two wisdom tooth having cavities needs to be extracted out as her equipment can't fill those teeth and they are slightly bent. On a fearful note I visited another dentist near by. He said my wisdom teeth do have cavities but he can fill them up and they are straight. Apart from that the rest of my teeth are absolutely alright. My question, in this situation what shall I do? And as a matter of fact I never visited the dentist because my wisdom teeth were a problem, I visited because of another tooth. What shall I do now? Can I reverse these cavities naturally at home? I am just 23 years old and am afraid of this tooth extraction and fill up. I dont know what will happen to this teeth and the rest down the lane.... Please help me. —gayatri
Often different dentists will have different opinions of what should be done. These opinions differ based on the philosophy and education of the dentist. Regarding wisdom teeth, some dentists prefer to extract them rather than fill them because they are difficult for patients to keep clean and they can create more problems later because of this. Very shallow decay can be reversed but if your dentist recommended fillings or extractions then it is very unlikely that they can be reversed. In most situations I would recommend extracting wisdom teeth rather than filling them but it also depends on how healthy your gum tissue is around the wisdom teeth. I suggest you find a dentist you feel comfortable with and talk about all your options, ask questions like " what can I expect over the next 10 years if I choose to not have my wisdom teeth extracted?" This should open up a good line of communication for your to get the answers you need to make a well informed decision.
-Dagon Jones
2016-09-25 17:35:37 I had two implants done in May 2016 by a Dentist that my regular Dentist recommended me to. Afterwards I saw my regular Dentist and on my last visit to him last week (September 22) he made some incisions with an instrument that cut and sort of burned my gums. My gums are still very painful. What is the instrument he used and is that a normal step in the procedure? —Shar004
It is very normal for the tissue around an implant to need to be adjusted. This is often done with a scalpel, or a laser, or an electrosurgery instrument. The last two cauterize the tissue so it will leave a slightly burnt taste for a couple of hours after. Rest assured that what you had done is very normal. -Dagon Jones
2016-10-24 20:29:15 My upper front teeth are getting sensitive and I feel like my gum line is receding I'm going to the dentist but I want to know is this very serious and is there prevention methods I can do now to prevent it further —rkin
Recession can be caused by several factors. The most common are tooth brush abrasion, gum disease, and bruxism (clenching teeth). Minor recession is often not a large concern and it can lead to some sensitivity, try sensodyne toothpaste (which may help a little bit). You should see a dentist about what the cause is, as there are different treatment approaches to all of them. Make sure you are using a soft toothbrush and not using too much force when you brush- Dagonjones
2016-10-28 15:49:37 The short summary of my question is: can a dentist think a filling would be sufficient to fix decay in a tooth from an X-ray but once they start drilling, realize they need to a put a crown in instead? For some context. I recently was forced to change insurance, and my previous dentist wasn't in network under the old plan. I went to my new dhmo dentist, and after a clean bill of health last year, my new dentist says I need 4 crowns replaced and 8 fillings. I was suprised, so I got my X-rays and got a second and third opinion from 2 of my old dentists. They said I did not need this much work done, have some decay that need to be repaired in my number 8 tooth asap. He said the tooth didn't show any decay last year, and was suprised by how aggressive the decay has been. This tooth,number 8, has a veneer after it broke when I was younger, , and my number 8 tooth needed a root canal 3 years ago as well. I have expensive veneers on both of my front teeth. The second opinion thought the decay needed to be repaired soon, and thought a filling would be able to fix the problem. My assigned dentist wants to take my veneers off that tooth, and put on a crown which wouldn't look as nice. Since I have veneers on my other front tooth that broke, she wants to take Veneers of both teeth, and put a crown on that healthy tooth so both of my front teeth match. I would like to go back my assigned dentist and ask her to just put a filling in my #8 tooth. 1. Would my very busy dentist be resentful of me questioning her judgement and not do a good job with the filling? 2.Is it possible my second opinion dentist is unable to determine the amount of decay without getting into the tooth, and if my assigned dentist we're to start to drill, she could decide there's too much decay for a filling and would need to put a crown on my number 8 tooth, and my other front tooth as well.? I'm really nervous about this scenario. not only about the costs associated with new crowns on my 2 front teeth , but that they won't look as nice as the veneers I currently have on as well. Im not sure the material he is using. But my insurance and I will only pay for 130 dollars for that crown. I appreciate your help —Kevin4949
The short answer is yes, sometimes the x ray does not show the whole picture. Once you clean out the decay you may find that a different restoration is required. I can't really say if one dentist might be resentful or not, that is a matter of personality. If they would then do a poor job on your dental work because they were resentful would make them a very poor practitioner in my opinion. The bottom line is you should go to a dentist you trust, I would not receive dental treatment from someone who's opinion I did not have faith in. -DagonJones
2016-11-24 10:22:04 Hope you guys can help. About 2 months ago, I went to the dentist and he did root canal. I went back for the second part, and there was no problems. I noticed a few days afterwards that there was a lump on the gum under the tooth in question. I asked my dentist and he told me not to worry. The thing is it seems to get bigger and the goes back down every now and again, its painful to touch, but the tooth itself is fine. What should I do??? —cole75
Talk to your dentist, you may benefit from some antibiotics but this type of situation can occur after a root canal and it just may need time to heal. DagonJones
2017-01-09 08:54:20 How do they fix a cracked tooth —beth225
2017-01-09 09:01:02 How do they fix a cracked tooth? Apparently my dentist didn't have time for me today and I'm getting upset because I don't want a crown on my tooth. They said they have to take the filling out to see if it is a small or medium or large crack in my tooth I'm scared 😳 out of my mind about this and hate getting numbed by a shot in my mouth 😞 —beth225
Yes, that is what has to be done, the filling often needs to be removed before one can tell if it needs a crown. I think this is a sign of a good dentist because they are being very thorough, and carefully evaluating the situation, instead of just deciding to do a crown because they suspect a fracture. -DagonJones
2017-01-18 10:58:18 I had a crown (no root canal) put on 3 months ago. My dentist needed to install a pin in the stump prior to crown placement. When he inserted the pin I experienced a very sharp pain that refuses to go away. The intensity of the pain varies and seems to increase with usage of the tooth. My dentist seems to be at a loss as to what is causing this pain. There is only minor pain when he taps on the crowned tooth. Your input is appreciated. Thank you. —flultiehopkins
I am sorry to say but that is a very hard question to answer without more information. A pin could refer to a small retaining pin or a large post that goes into the root canal treated space of a tooth. I would need to see an x ray to tell you more. -DagonJones
2017-03-02 21:44:05 Hi Dr. Jones, Eric Jensen, one of your former patients. I am having some dull, intermittent pain in my lower right molar (#17) for a few weeks now. It will hurt for a little bit on and off for a few days, a few days will go by with no pain, and then the pain will come back again. I asked my current dentist about it a month ago when I went in for another issue (a follow-up appt for a gum graft in the same quadrant, performed in late December last year) and she looked at my most recent x-rays (which were taken last mid-December). She said that everything looked ok and that she didn't see any decay or other problems. I am not experiencing too much pain but still things don't feel quite right. Perhaps there has been some decay since last December? Perhaps this is my gum graft still healing? On this tooth I have a large metal filling and when I feel it with my tooth it feels quite rough and sharp--I have one or two other molars with fillings that feel much smoother. I plan on calling and making another appt tomorrow, but am also curious as to what you think. Thank you so much! —EricJensen
Hi Eric, I hope you are doing well. What you are experiencing s likely nothing to worry about. Perfectly healthy teeth can sometimes have dull intermittent sensitivity. This is likely the result of some chewing or grinding pressure on the tooth. The ligament that houses the tooth in the bone can become a little irritated and ache on and off. As long as the pain is not intense and throbbing you likely have nothing to worry about. Decay in the tooth will not likely cause any pain unless it is very very deep and that would take a year or two to get that way. It is possible that there is a fracture on this tooth but that would typically present as sharp pain every time you bite down and that does not sound like your symptoms. Because you recently had a gum graft here this area is a bit more likely to experience sensitivity. _Dagon Jones
2017-03-18 16:16:56 Dr. Jones, thank you so much! You are one of a kind. I appreciate your comment as it gives me much comfort. Thank you, Eric —EricJensen
2017-04-09 13:40:33 I was recently to the dentist a few months ago and I was told by the dentist that my most logical option was to have all my teeth pulled and get dentures. Now I know I have gingivitis as well as I feel deep in my guts there Is something bigger going on wrong with my teeth/mouth/throat. I was wondering how many mouth diseases are associated with teeth? And what they look like? As well as What things could also be wrong with my mouth if you had to guess? As I said there really bad I have gingivitis, my teeth kill my jaw bone in sharp breathtaking shooting pain to my head. my teeth are so decayed one side the upper right jaw has been evicted of all my teeth minus one so there all really bad too. the infection is so bad that 4 times of antibiotics including doeses that is not recommended for people who are not seriously in harms way still were not helping. As a child I ate a lot of sugar and was moving around so much that I didnt really brush my teeth alot, and I ate alot of acidic food, I did several really bad drugs that rotted my teeth quicker than anything ive done, and drank alot. So I know i did this to my poor teeth and mouth. I regret it now and havent gotten all my teeth pulled the day I was supposed to go get them all pulled out was just after my 25th birthday in feb, I got scared and didnt go. They were gonna just keep me awake and just numb it but most of the time on one simple extraction the numbing doesnt fully work so the thought of having them pull them all out with just the numbing really freeked me out cuz I am scared of the mouth pain as is I mean it couldnt get much worse. I just wanna know what could be wrong before I go back to the dentist! —torisidy
There are several health conditions that can effect the teeth but almost all of these have very significant whole body symptoms that would be much more significant than any dental issues. If you any of these conditions you would likely have significant medical problems with your bones. You probably have significant periodontal disease and decay. Periodontal disease effects the bone and structures that hold the teeth in the gums, over time these structures are destroyed by peridontal disease. Periodontal disease and decay will continue if left untreated. There are strong links between periodontal disease and other health conditions such as diabetes and heart disease so I think it is important that you do get comprehensive treatment. Extraction of all your teeth may be the best option, extraction of the teeth with local anesthetic is often the best option and can be done with very little discomfort. Make sure you tell your dentist about all your fears, they may be able to give you some medication to help relax you. You probably do not have any other significant health problems that are causing your tooth problems, it sounds like a lack of dental care is the source of the problems. Don't worry, you are not alone, many people are in the same situation as you are, listen to your dentist, talk to you dentist about your concerns, and you will likely be much better off if you get the care that is recommended.- Dagon Jones
2017-05-11 11:20:23 I had a cracked molar, upper left, which was not causing me any problems whatsoever, but my dentist said that I should get it filled. It also had a little bit of decay. So in early December 2016 I had the recommended filling done. It's a composite resin. Ever since then, I have had pain in the tooth when chewing or biting and pain in that tooth when flossing. She has made bite adjustments four times, and filed down the filling that went up the side of the tooth between it and the tooth in front of it. There is no tooth behind it. . After the fourth adjustment not resolving it, she sent me to an endodontist for evaluation, saying it could be irreversible pulpitis. He examined me, and determined it's not irreversible pulpitis. He said the filling is small. The pain seems to be when I bite down, not upon release of the bite. He said cracked teeth are unpredictable, what usually works fine on many people will fail for others. Just my bad luck. She never said anything like this! He recommended putting on a temporary crown for a month, and if that resolves the pain issues, then put on a permanent crown. If it doesn't resolve with the temporary crown, then it's a root canal then permanent crown, but the tooth still might not be able to be saved. I switched to a new dentist, as I've lost confidence in her, plus she's not participating in my dental insurance network, which would cost me a LOT more money with all this expensive work I now need. My new dentist said the same as the endodontist. I needed a crown lengthening procedure, which I had last week. I got the temporary crown yesterday. I figure it'll be a couple days before I can see if this has helped. Right now it's still sensitive from all the grinding to prepare it for the temporary crown. I'm wondering if maybe when she was drilling on the tooth it caused the crack to get worse? It's especially frustrating because this tooth was pain free until I got this recommended work done. I'm also upset that she didn't tell me that a cracked tooth can respond unpredictably to treatment. Did she not know this? Why did she let this go on and on? I've been chewing almost exclusively on the right side now for almost 5 months, and now the bottom right molars are somewhat sensitive to chewing pressure. This has really affected how and what I can eat. At first, massaging the masseter muscle on the right side helped. I'll try doing the massage more, but I'm really hoping that when I can chew on the left side normally again the sensitivity on the right side will resolve. If I could go back, I wouldn't get that filling. I'd wait until there was an issue, then get a crown. —Dhammagirl
When the filling was first done it could have made the symptoms of the crack worse, however, if nothing was done then the decay would have progressed over time destroying more tooth structure and putting the tooth at more risk. I think your first dentist did the right thing by putting in a filling. Any time you are dealing with a biological system there are unpredictable factors that can not always be accounted for. I can not say what your first dentist knew or what she thought the risk factors were but I assume she probably thought that the risk of the fracture getting worse was very very small and therefore simply did not mention it as a risk. I am familiar with the situation you are describing and it is very uncommon but it can happen. The treatment you are receiving the the recommendations you were given sound like very good, conservative treatment options. I understand that you are frustrated by the lack of warning you received about this risk but it is very likely this whole thing would have happened if you had chose not to do the filling in the first place. - Dagon Jones
2017-05-19 12:46:14 I had a stainless steel crown put in in February. It hurt when I bit into hard food, so I went to the dentist and she filed a bit of this risk is very small then he crown down. It's a little scratchy but doesn't bother me. I'm worried though cause I read online that scratching the crown may lead to corrosion . Do I have anything to really worry about? Is this crown likely to corrode or release toxic ions? —Jlo
If it is stainless steel it is very unlikely to corrode, if it does corrode it would not produce any toxic ions. Stainless steel crowns are intended to be temporary and should be replaced with a permanent custom crown within about 5 years. -Dagon Jones
2017-06-17 11:36:38 Hi Dr, Jones, I have a dental implant to replace a permanent tooth that never grew in-its the right eye tooth (#7?). In researching the safety of the materials used to make the implant, I found a great deal of information on the perceived safety of titanium, and was relatively satisfied with this. I was not informed that my implant was actually an alloy, containing aluminum and vanadium as well, until after it was placed.. I have a problem with this, the aluminum specifically, as it is a known neurotoxin, and I'm very young. I don't feel I was given the opportunity to give full consent, as I was never fully informed, and feel that my rights as a patient have been violated. I never would have had the implant placed had I known there were 2 other toxic metals involved. I'm very disappointed and honestly quite fearful about the potential longterm consequences of ion release, accumulation in the tissues, and toxicity. I need to have it removed. Are there surgeons who specialize in removal of integrated implants? —DeeDee
Pretty much any oral surgeon will be able to remove the implant. I don't think you have anything to worry about there though. The trace amounts of aluminum and vanadium in the alloy will not be released into your system. I am no expert on this by my understanding is that there would have to be some significant corrosion of the implant for metal ions to be released and these types of alloys form a very stable oxide layer that will prevent corrosion. -Dagon Jones
2017-07-12 01:07:03 I am 71 year old male. Diabetes 2. Dialysis 2 times per week. etcetera. I discovered 4 teeth (upper left that became soft and started falling apart.. Or so it seemed. What I discovered was all four teeth were cut through at the botton and from top to bottom down the middle. There is a medal rod in all four that is run into the jaw bone. Then a medal band wrapped around all 3 or 4 .. I assume to hold them in place. Plus a rod run through the teeth. What in the world did the dentist do? I've never heard of such a thing. What is even more mysterious is, I HAVE NO MEMORY OF THIS TREATMENT. NONE. I know I never paid for this work. It could have been done anytime between 1967 and 2011. I did show the loose rods and band to a dental who just shrugged her shoulders and moved on. I could go on. Can somebody tell what this is. It sounds like major work. —Chelan97
I am sorry but I just cannot give you any advice without seeing x rays and doing a more detailed exam. I can not make sense of the work based just on your description. -Dagon Jones